23 NATIONAL CONFERENCE\OCT. 8-10, 2023\PHX A SIPC PUBLIC A TION SIPCONL I NE.N E T OCTOBER 2023
Get the peace of mind and support it takes to self-fund your healthcare.
Self-insuring your healthcare benefits can open up new possibilities for your business — affording you greater flexibility in how you manage your healthcare spend. Trust the expert team at QBE to tailor a solution that meets your unique needs.
We offer a range of products for protecting your team and assets:
• Medical Stop Loss
• Captive Medical Stop Loss

• Organ Transplant
• Special Risk Accident
We’ll find the right answers together, so you can stay focused on your future.
New captive offerings now available!
Chat with us about how leveraging captives can help your business reduce healthcare costs.

 Matthew Drakeley Vice President, Specialty Markets
Matthew Drakeley Vice President, Specialty Markets
QBE and the links logo are registered service marks of QBE Insurance Group Limited. ©2023 QBE Holdings, Inc. This literature is descriptive only. Actual coverage is subject to the terms, conditions, limitations and exclusions of the policy as issued. Crop Specialty Commercial
We’ll focus on risk, so
take
of
Accident & Health Market Report 2023 Visit qbe.com/us/ah
you can
care
your business Accident & Health Insurance
4 SIIA ENDEAVORS: ON THE RECORD WITH SIIA PRESIDENT & CEO MIKE FERGUSON

13 ELATION AND FEAR OVER AI FROM MUNDANE TO CREATIVE TASKS, ARTIFICIAL INTELLIGENCE IS REVOLUTIONIZING SELF-INSURANCE, BUT CONCERN PERSISTS ABOUT VEERING OFF COURSE, THE IMPACT ON JOBS AND CYBERSECURITY
 By Bruce Shutan
By Bruce Shutan
49 ACA, HIPAA AND FEDERAL HEALTH BENEFIT MANDATES
THE AFFORDABLE CARE ACT (ACA), THE HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT OF 1996 (HIPAA) AND OTHER FEDERAL HEALTH BENEFIT MANDATES
66 NEWS FROM SIIA MEMBERS
The Self-Insurer (ISSN 10913815) is published monthly by Self-Insurers’ Publishing Corp. (SIPC). Postmaster: Send address changes to The Self-Insurer Editorial and Advertising Office, P.O. Box 1237, Simpsonville, SC 29681,(888) 394-5688
PUBLISHING DIRECTOR Erica Massey, SENIOR EDITOR Gretchen Grote, CONTRIBUTING EDITORS Mike Ferguson and Ryan Work, DIRECTOR OF ADVERTISING Shane Byars, EDITORIAL ADVISOR Bruce Shutan, 2023 Self-Insurers’ Publishing Corp. Officers James A. Kinder, CEO/Chairman, Erica M. Massey, President, Lynne Bolduc, Esq. Secretary

OCTOBER 2023 VOL 180 WWW.SIPCONLINE.NET OCTOBER 2023 3
TABLE OF CONTENTS
FEATURES
ARTICLES
43 NAVIGATING COVERAGE FOR WEIGHT LOSS MEDICATIONS 22
PAIN POINTS
EMPLOYERS 35 COSTLY WEATHER EVENTS FUEL CAPTIVE INTEREST
SPECIALTY PHARMACEUTICALS REMEDY
FOR SELF-INSURED
SIIA ENDEAVORS
ON THE RECORD WITH SIIA PRESIDENT & CEO
MIKE FERGUSON
TheTSelf-Insurer Editor Gretchen Grote sat down with SIIA President & CEO Mike Ferguson for a wide-ranging interview to talk about how the association continues to evolve and play an increasingly important role in helping its members be successful in the self-insurance marketplace.

ENDEAVORS
Mike Ferguson, SIIA President & CEO
4 THE SELF-INSURER
GG: Now that we are in the fourth quarter, how would you describe the year SIIA has been having so far?
MF: I am very pleased with how 2023 has been playing out from a SIIA leadership perspective. We had great participation in each of our in-person events as well as webinars for the first half the year, which is a great indicator of the vibrancy of any organization.
The association’s volunteer committees and task forces also met regularly to work on a variety of projects in support of SIIA’s mission to protect and promote the business interests of companies involved in the self-insurance/captive industry.
Of course, we always look at membership numbers as an important datapoint and I am pleased to report that the trend lines continue to be positive with new members being added every month. And these new members represent every segment of our industry.
GG: Since this is the National Conference edition of the magazine, would you like to highlight anything in particular about this event?
MF: Well first, we are excited to be back at the JW Marriott Desert Ridge, which is a favorite location with our members based on feedback received.
As we talk here today, the registration numbers look very strong so it’s possible that this year’s conference will be the biggest SIIA event ever.
But regardless of the final attendee count, our team has put together a really great program, combining top-notch educational content with multiple networking events.
We are particularly looking forward to the keynote presentation by Futurist Mike Walsh who will be talking about how we should be preparing our businesses to take advantage of the latest advancements in artificial intelligence. And of course, we have another great conference party planned to cap everything off.
GG: How has SIIA’s educational event strategy evolved and what should members expect for 2024?
MF: Over the last three years, we have identified opportunities to
develop targeted educational content and related networking environments that provide value to our members and created new events to deliver this value.
These events have included the Health Price Transparency Forum, Future Leaders Forum and Corporate Growth Forum. All had year-over-year attendance growth in 2023 and will be back on the calendar for 2024.
Our inaugural Cell & Gene Therapy Stakeholder Forum was so popular this year that it was actually sold out, so it will also be back next year with more space! Consistent with this successful approach, we have created yet another new event for 2024 focused on Artificial Intelligence, which we believe will be very well-attended. AI is coming to every other industry so we shouldn’t expect to be an exception.
Finally, we are exploring the possibility of bringing back our International Conference for later next year for those companies looking outside the United States for business development opportunities and risk management solutions.
We are planning for a very busy year so please be on the lookout for an event calendar, which will be published soon if not already.
ENDEAVORS
OCTOBER 2023 5

Is your payments solution delivering more to your bottom line? Expect more with ECHO® echohealthinc.com
GG: SIIA has had a busy and successful year on the advocacy and policy front. What should members know and how can they engage?
MF: This year has been extraordinarily busy, and SIIA continues to be at the forefront of educating, protecting, and growing our industry before policymakers and regulators.
On the federal side, we were able to pass the Self-Insurance Protection Act in the U.S. House and continue to help forge legislation to increase price transparency and bring more clarity and data sharing to the Gag Clause provision.
Bringing sunlight to these areas of healthcare costs leads to successful and affordable selfinsured plans for employers and plan participants. On the regulatory side, we have filed

comments on captive insurance regulation, in addition to engaging in current proposals related to health insurance and mental health.
On the state side, SIIA was successful in pushing back on stop-loss regulation in Rhode Island, a small group prohibition proposal in New Jersey, and engaged in Nevada as the regulators there crafted a new small group regulation.
SIIA member engagement starts with communication and education, in addition to participation in the Self-Insurance Political Action Committee. Members communicating with the SIIA team, and with policymakers and educators, about not only the role our industry plays, but the opportunities and challenges that are before us is essential. Education, relationships, and ongoing communication are the foundation of a strong advocacy platform.
GG: Let’s talk more about SIPAC. You have commented publicly on several occasions about how important it is for SIIA to become more of a major player in terms of political contributions. Can you elaborate a bit on why this should be such a priority and give any progress that has been made to move in this direction?
MF: I have been saying this for the past several years and this objective has continued to move up the list of association priorities.
There are two primary reasons for this emphasis, with the one reason being fairly obvious for most members, with the second reason less
Subrogation Management
At Davies, we provide thorough investigations and subrogation support specifically tailored to all classes and entities within the insurance sector.

Reach out for more information on how we can help your insurance business.
 Marie Noble, MBA, AIC VP of Subrogation Management Marie.Noble@us.davies-group.com
Marie Noble, MBA, AIC VP of Subrogation Management Marie.Noble@us.davies-group.com
davies-group.com/us
ENDEAVORS OCTOBER 2023 7
Complete, customizable TPA solutions
From locally-focused to national-scale programs, AmeriHealth Administrators offers a full spectrum of third-party administration and business process outsourcing services. Our scalable capabilities service many unique customers, including self-funded employers, Tribal nations, international travelers, and labor organizations.

We offer innovative solutions, insight, and expertise to help you manage your health plan and capabilities, control costs, and support employees’ health.
Visit amerihealth.com/tpa
to learn more about how we can work with you.
obvious for those who are not creatures of the DC lobbying world.
The obvious reason, of course, is that it is much easier to make and keep friends on Capitol Hill if you provide financial support for their campaigns. This does not mean that if you contribute to a specific member of Congress that they are certain to vote a specific way, but it’s certainly easier to get a meeting with the member and/or their senior staff to explain your issues.
Not so obvious to those outside the beltway is that when an organization establishes itself as a political financial player, it raises your “street cred,” so to speak, with other important organizations in town that we may need to partner with on various lobbying efforts.
Our progress has been somewhat slow but steady since we established the Self-Insurance Political Action Committee (SIPAC) about eight years ago as a vehicle for SIIA members to channel political contributions to key members of Congress.
Things have accelerated over the past few years thanks to this more dedicated focus, combined with increased staffing resources, and you are now starting to see SIIA really establishing itself as a money player in DC.
Obviously, we are not the biggest name by any means, but it’s solid progress that has already directly complimented advocacy efforts and we expect even more positive results after the upcoming election.
GG: I very recently have seen that SIIA has participated in several important court victories. What do those mean and what should members know?
MF: SIIA has a long history leading and participating in larger coalition efforts on the legal front to support our members. We couldn’t do this without the association’s Legal Defense Fund (LDF), which in turn is funded by voluntary contributions from our members.
This year alone, SIIA has participated in four separate amicus filings related to surprise medical billing, seeking to ensure that the negotiation and arbitration process is fair for patients and plans. The legal fight over the No Surprises Act is ongoing, but it’s an important one in the face of legislative uncertainty.
More recently, multiple states have undertaken efforts to erode ERISA’s preemption powers through PBM legislation enacted in the wake of the U.S. Supreme Court’s Rutledge decision.
Just a few weeks ago, the 10th Circuit Court agreed with an amicus that SIIA participated in, finding that an Oklahoma PBM law restricted a selfinsured plan sponsor’s ability to develop provider networks and other value-based plan designs intended to lower costs.
SIIA continues to be active in supporting ERISA preemption legislatively, as well as through legal channels where necessary.
GG: It seems like the SIIA look has been more polished this year, can you tell us anymore about that?
MF: Yes, that is correct. We were fortunate to be able to add a senior marketing and communications professional to our team at the beginning of the year and one of his priorities has been to help polish the SIIA brand.
This work has taken place over the last several months with improvement in the quality and consistency of our external communications. A broader strategic branding campaign is also being developed for launch early next year. SIIA has a great story to tell, and we look forward to telling it more effectively in the coming months.
ENDEAVORS OCTOBER 2023 9
GG: How is the SIIA Future Leaders initiative coming along?

MF: Let me first say that this remains one of the association’s most important strategic initiatives as the generational shift continues to accelerate in our industry, so I am pleased to report that things are going great. Activities are now guided by a very active Future Leaders Committee, so we are confident that this member service offer matches the needs and interests of this targeted demographic.
Our Future Leaders Forum earlier this year was a big success with young professionals attending
from around the country. We even held a first-ever SIPAC Future Leader fund-raiser event in conjunction with the Forum that was very popular.
Many younger members also participated as part of a virtual Mentor Connect event, which matched them with senior industry executives for small group career coaching discussions.
I know more good things are in the works for our younger members and we look forward to making more announcements soon.
GG: The association continues to see an increase in its captive insurance membership constituency, so how do you view SIIA’s role in this segment of the marketplace?
MF: My view is that SIIA continues to play a unique and useful role in the captive insurance space by integrating its stakeholders into the much broader self-insurance world.
This is important because mid-market employers are becoming increasingly sophisticated in how they manage risk, understanding

® 10 THE SELF-INSURER
ENDEAVORS
that they can integrate multiple self-insurance strategies that may include the formation of a captive insurance company. SIIA brings this all together, giving captive insurance professionals more educational, networking and advocacy resources.
I am particularly pleased to see how much progress SIIA has made over the past year with political advocacy in Washington, DC to better position the captive insurance market segment with key policymakers.
Most recently, our captive insurance company developed a survey for industry stakeholders in an attempt to collect important data that has not been available previously. Second year survey results are expected to be reported soon, which I believe will be very valuable for SIIA members and others.
GG: There certainly sounds like a lot of exciting things going on at SIIA. What advice would you give industry executives who want to become more active in the organization?
MF: Well of course, become a member if you are not already. Showing up at association events - as they are available - is a big deal because SIIA is a very interactive and social organization and there is no substitute for being there.
We also recruit members to serve on our various volunteer committees and participate in periodic grassroots lobbying campaigns, which are great involvement opportunities, so watch for periodic volunteer recruitment communications. I like to say we are happy to put our members to work!
For more information visit www.siia.org.
Do you aspire to be a published author?
We would like to invite you to share your insight and submit an article to The Self-Insurer! SIIA’s official magazine is distributed in a digital and print format to reach 10,000 readers all over the world.
The Self-Insurer has been delivering information to top-level executives in the self-insurance industry since 1984. Articles or guideline inquires can be submitted to Editor Gretchen Grote at ggrote@ sipconline.net
The Self-Insurer also has advertising opportunties available. Please contact Shane Byars at sbyars@ sipconline.net for advertising information.

ENDEAVORS
OCTOBER 2023 11
Somebody has to come in second. Make sure it’s not you.
There are no insurance MVP trophies, no best PowerPoint awards, no fantasy broker leagues. You show up first with the best option for your client, or you lose. We never take this for granted. That’s why we leverage all of our people, data and relationships to reach one goal: We help you win.
We help you win.
ELATION AND FEAR OVER AI
 Written By Bruce Shutan
Written By Bruce Shutan
Everyone is talking about both the promising and alarming impact of artificial intelligence – from office water coolers to kitchen tables. Those conversations – which are also on the agenda at SIIA’s 2023 national conference this month – have intensified over new “generative” AI applications such as ChatGPT that produce text, images or other media.
For self-insurance, there are a myriad of possibilities. From laborintensive to creative tasks, AI can be used in a number of areas. They include automating patient intake; scrubbing or updating patient data in electonic medical records; identifying high-quality providers; customizing population health strategies; improving triage, treatment and outcomes; bolstering predictive modeling; and suggesting actionable items.
FEATURE E
OCTOBER 2023 13
From mundane to creative tasks, artificial intelligence is revolutionizing selfinsurance, but concern persists about veering off course, the impact on jobs and cybersecurity
Those are tall orders for a technology that the industry perceives as potentially game-changing. There’s now an expectation, for instance, that pre-authorizations can be immediately turned around, according to Brian Wetter, vice president information technology, infrastructure and analytics at PacificSource Health Plans who will take part in a SIIA panel discussion in Phoenix on how AI is affecting TPAs.

Adoption of this technology is considered necessary for success, according to Matt Salerno, a software architect for VBA who also will speak about AI at SIIA’s conference. “The integration of traditional machine learning and generative AI within the health care and TPA space will become not just a value-add but a necessity,” he believes. “Those that adopt it will succeed and thrive, while those that do not will fail or be acquired for their book of business.”
PILOT TO CO-PILOT
AI’s role is that of a copilot or thought partner helping manage someone’s workload so they can focus on their core competencies and be more strategic, Wetter observes. He recently turned to AI for help crafting a presentation to the board that required a short paragraph defining self-funded administration, which he tweaked in only about 30 seconds.
Another common use involves his firm’s RFP software, which is integrated with ChatGPT and is trained to recognize historical RFP responses. “We’ll get a question, ‘can you deliver any [electronic data interchange] 834 file to a customer?’” he notes. “It’ll generate the response and it is spot on. It is exactly how we would respond to that question.”
That’s not to say every interaction will go smoothly. At a time when this nascent technology is producing strange and threatening responses to freeflowing conversations, Wetter admits that generative AI lacks enough context to confidently answer many other questions and may send responses that essentially mirror a hallucination.
Wetter believes the mundane part of administering selfinsured health plans is where AI is actually poised to deliver the most value. For instance, it recently red-flagged a client’s allergy claims involving scratch testing and injections that showed one provider in particular building in an additional code that none of the others charged.

But there’s a larger context to these capabilities. PacificSource Health Plans uses a proprietary algorithm that prescribes programs for members with whom they engage in active outreach. A concerted effort is made to fully understand each patient’s clinical history, local provider resources and social determinants of health.
he explains.
“That’s a prime example of how we’ll see AI come into play to help make better decisions faster.”
14 THE SELF-INSURER
“These are not traditional things that you would hear from an administrator,”
Brian Wetter
Elation and Fear Over AI
Matt Salerno
“You have become a key partner in our company’s attempt to fix what’s broken in our healthcare system.”
- CFO, Commercial Construction Company
“Our clients have grown accustomed to Berkley’s high level of customer service.”
- Broker
“The most significant advancement regarding true cost containment we’ve seen in years.”
- President, Group Captive Member Company
“EmCap has allowed us to take far more control of our health insurance costs than can be done in the fully insured market.”
- President, Group Captive Member Company
“With EmCap, our company has been able to control pricing volatility that we would have faced with traditional Stop Loss.”
- HR Executive, Group Captive Member Company
People are talking about Medical Stop Loss Group Captive solutions from Berkley Accident and Health. Our innovative EmCap® program can help employers with self-funded employee health plans to enjoy greater transparency, control, and stability.

Let’s discuss how we can help your clients reach their goals.
This example is illustrative only and not indicative of actual past or future results. Stop Loss is underwritten by Berkley Life and Health Insurance Company, a member company of W. R. Berkley Corporation and rated A+ (Superior) by A.M. Best, and involves the formation of a group captive insurance program that involves other employers and requires other legal entities. Berkley and its affiliates do not provide tax, legal, or regulatory advice concerning EmCap. You should seek appropriate tax, legal, regulatory, or other counsel regarding the EmCap program, including, but not limited to, counsel in the areas of ERISA, multiple employer welfare arrangements (MEWAs), taxation, and captives. EmCap is not available to all employers or in all states.
Stop Loss | Group Captives | Managed Care | Specialty Accident ©2022 Berkley Accident and Health, Hamilton Square, NJ 08690. All rights reserved. BAH AD2017-09 2/22 www.BerkleyAH.com
The technology is also helping identify health plan members who haven’t seen their primary care physician two weeks after an emergency room visit or prime candidates for surgery in the next 12 to 16 months, observes Michelle Bounce, president of the


J.P. Farley Corporation, another AI panelist at SIIA’s conference.


But there are limits to what AI or generative AI can do. For example, she says what’s lacking is a good weighting system for gauging quality. While clinical pathways can be built into AI and create alerts when they’re not being followed, she explains that their value depends on several factors (i.e., a nuance not being followed, wrong clinical pathway or physician not following the pathway). Making these determinations could help improve weighted quality scoring.
Like payment-integrity systems, AI also can be used to detect fraud, waste and abuse on labor-intensive, high-dollar claims, as well as review appropriateness of care, according to George Stiles, president and chief operating officer of Planned Administrators, Inc. who also will speak about AI at SIIA’s conference.
His firm is focusing on large hospital claims. In sifting through medical data, the aim is to determine if claims were correctly coded and billed. “What we’re finding is that there’s a whole lot of stuff going on in that $10,000 to $20,000 claim range that’s just been flying under the radar up until now,” he reports.
16 THE SELF-INSURER For product information, contact: marketing@amalgamatedbene ts.com Amalgamated Life Insurance Company Medical Stop Loss Insurance— The Essential, Excess Insurance Amalgamated Family of Companies Amalgamated Life ▲ Amalgamated Employee Benefits Administrators ▲ Amalgamated Medical Care Management ▲ Amalgamated Agency ▲ AliGraphics Group • Stop Loss • Voluntary Amalgamated Life Insurance Company 333 Westchester Avenue, White Plains, NY 10604 914.367.5000 • 866.975.4089 www.amalgamatedbenefits.com As a direct writer of Stop Loss Insurance, we have the Expertise, Resources and Contract Flexibility to meet your Organization’s Stop Loss needs. Amalgamated Life offers: VOLUNTARY SOLUTIONS—KEEPING PACE WITH TODAY’S NEEDS • Accident • AD&D • Critical Illness • ID Theft • Dental • Disability • Hearing • Whole Life Insurance • Specialty Rx Savings Programs and Discounts • “A” (Excellent) Rating from A.M. Best Company for 47 Consecutive Years • Licensed in all 50 States and the District of Columbia • Flexible Contract Terms • Legal • Portable Term Life • Excellent Claims Management Performance • Specific and Aggregate Stop Loss Options • Participating, Rate Cap and NNL Contract Terms Available Policy Form ALSLP-2020* *Features & form numbers may vary by state. A M BEST S A Exce en Financ a St eng h Ra ng Michelle Bounce Elation and Fear Over AI
Mindful that younger people who are coming into the workforce are more adept at using chat text vs. actually talking to someone, Planned Administrators, Inc. has embraced AI from a customer-service standpoint. One employer client is using AI to do member navigation, helping individuals find specialists based on an analysis of their claims data and quality metrics. The technology may recommend, say, the five best orthopedic surgeons in Atlanta for a 47-year-old female with certain diagnosis codes and comorbidities listed in her medical history. “It’s
A third point Salerno makes is that generative AI for technical integration will help health care organizations bridge the gap between different systems, acting as intelligent middleware. These models create interfaces that adapt in real time by understanding data structures, semantics and communication protocols. They also ensure smoother data flow and reduced system integration times, as well as a more holistic view of patient data across platforms for TPAs and other health care entities.
And where providers are concerned, the TPA realizes they want a quick and easy way to check eligibility or verify benefits, and would prefer to receive the information correctly from a chatbot than wait and talk to someone.
MOUNTING CAPABILITIES AND HIGH VALUE
Salerno predicts four major areas will emerge within the next five years that provide the most value to self-insured health plans and their partners. The first involves traditional machine learning that will take the form of enhanced adjudication. Systems will not only identify patterns and anomalies in claims submissions, but also be equipped to auto-correct potential errors. These capabilities would drastically reduce the manual labor and oversight that’s usually required in claims adjudication, resulting in reduced costs and improved efficiency.
Another noteworthy trend he sees involves smart-assistants built upon generative AI models that dynamically respond to user queries. They’re able to tap vast vector databases created from various knowledge bases such as user help systems, support tickets and customer or client resource centers. The expectation is that by offering dynamic and contextually relevant assistance, these aids will offer improved usability of claims administration software that results in enhance productivity and reduce training time for health plans and TPAs. Smart-assistants also can offer a more intuitive interface that anticipates user needs, automating various tasks from plan builds to workflow creation.
Finally, he notes that generative AI for organizational knowledge serves as a reservoir of institutional knowledge in the face of staff turnover. These models can provide insights, context and guidance to new members by training on organizational data, effectively simulating years of experience. Drastically reducing the impact of onboarding and training times will ensure that even newest team members can quickly make informed decisions. In addition, the health care industry benefits by maintaining consistent service levels and knowledge transfer across entities.

a very different list than if you just look at generic quality scores,” Stiles explains.
OCTOBER 2023 17
Elation and Fear Over AI
George Stiles

www.bhspecialty.com/msl A trusted business name. A stellar balance sheet. An executive team with 30 years of experience. Creative, tailored solutions. Berkshire Hathaway Specialty Insurance is proud to bring our exceptional strength, experience and market commitment to the medical stop loss arena. A medical stop loss grand slam. It’s a home r un for your organization. Atlanta | Boston | Chicago | Columbia | Dallas | Houston | Indianapolis | Irvine | Los Angeles | New York | Plymouth Meeting | San Francisco | San Ramon | Seattle | Stevens Point Adelaide | Auckland | Barcelona | Brisbane | Brussels | Cologne | Dubai | Dublin | Frankfurt | Hong Kong | Kuala Lumpur | London | Lyon | Macau | Madrid | Manchester | Melbourne | Munich Paris | Perth | Singapore | Sydney | Toronto | Zurich
INHUMANE TOUCHES?
Within the past year, fear is mounting that this technology will replace people and service, but Bounce says that’s a shortsighted assessment. “There are a ton of uses for AI in our industry, especially generative AI, where it involves the most risk and cost,” she says. One area that is ripe for usage is building out benefits, which can take years of experience to do.

Either way, the marketplace obviously must adapt to U.S. labor and demographic trends. People 35 and younger are only staying in a job for two or three years, which she notes “creates a significant risk to the sustainability of our industry that I think we have to acknowledge.”
The underlying problem, she explains, is that it takes time for people to become fluent in the self-insured industry. Given that fact, it’s best to redeploy workers to where they’re needed most, such as using generative AI to turn documents into plan builds or educating members to make better benefits decisions.
“I trust the technology to code better than people,” Bounce says. As for account management, which she notes is another job in this industry that takes years to learn, AI can adeptly handle the bits of analytics, price comparisons, actuarial underwriting and plan recommendation functions
that the work entails. Service providers in the self-insured space can’t keep people fast enough in the under-35 market to sustain the industry without creating depth with technology, she warns.
Bounce notes. That information should include actionable items, education, opportunities for direction or steerage. “We
While AI technology is generating tremendous excitement, it also raises serious concern about cybersecurity. Data on an opensource platform like ChatGPT may be vulnerable. In the absence of safeguards, Stiles has seen instances in which some data is easily
“If we put humans back into the equation, I think AI and AI generative are only going to make that interaction more valuable and more critical because what we’re going to end up getting is a whole lot of information coming at us at once,”
can’t forget that healthcare is a very human experience,” she adds.
OCTOBER 2023 19 Elation and Fear Over AI
accessed for all kinds of different analyses, filters and so forth. Spear phishing attempts also are a huge concern. Wetter says generative AI can detect anomalies in, for instance, the way emails are written to uncover “digital twinning,” which enables cyber attacker to impersonate individuals.
Whatever comes of this issue, Bounce sees both a dark and light side to AI. If the focus is on the service aspect being a centerpiece of this solution, she cautions that “we just go down the road further of dehumanizing the system, increasing the cost unnecessarily and forgetting who the customer is, and that has catastrophic consequences.
“The other side of this,” she continues, “is that we use it in a smart manner that allows us to minimize not just risk for us as the administrators, but also protect those clinicians who are being pulled
around by the hospital to not do what they believe clinically is in the best interest of the patient. It can go a long way in helping us with quality scoring, patient directives and education.”
Bruce Shutan is a Portland, Oregon-based freelance writer who has closely covered the employee benefits industry for more than 30 years.
OCTOBER 2023 21 Elation and Fear Over AI
SPECIALTY
PHARMACEUTICALS: REMEDY PAIN POINTS FOR SELF-INSURED EMPLOYERS
Written By Laura Carabello
There’s
Tno doubt that employers are still reeling with the introduction of novel, expensive and potentially lifesaving cell and gene therapies, but they must also prepare themselves for the relentless launch of specialty medications and infusion therapies that are on the horizon.
The significant impact of the drugs on budgets and benefits planning cannot be underestimated, and while new weight loss drugs are not typically classified as specialty drugs, they are already adding yet another layer of cost.
Easing the strain and impact of these specialty pharmaceuticals requires thoughtful strategies as their sheer number and scope challenge even the most astute employers to improve patient

FEATURE
22 THE SELF-INSURER
access to treatment while ensuring affordability. In the year ahead, targeted programs, financial solutions, and other initiatives to relieve these stinging issues necessitate the guidance of professionals.
Thanks to SIIA, attendees at the 2023 National Conference will get this much needed direction from three highly credible industry thought leaders, Monday, October 9, 2023, 3:15 to 4:30 PM.
• Dea Belazi, CEO, Ascella Health
• Corey Belken, Senior Employer Account Executive, Genentech, Inc.


• Dr. Brenda Motheral, CEO & Co-Founder. Archimedes.
ISSUES, TRENDS AND SOLUTIONS WORTH WATCHING IN 2023-2024
Dea Belazi says, “Emerging and continuing issues are being seen with specialty drugs in the year ahead. While specialty drugs are costly, they also can provide life-changing options to physicians and patients. A key issue is the continuing affordability of these products and employers will need to balance cost and access to ensure optimal patient outcomes. In 2022, the median annual cost for newly approved drugs was greater than $222,000 and high cost will continue to be a significant barrier to access.”
He points to reports that almost half of specialty pharmacy patients have experienced challenges in receiving specialty medications, with nearly a quarter of these patients stating high medication costs as the top challenge in gaining access.
Belazi. “Innovative financial solutions for CGT are now available amid continued increases in CGT costs that are putting pressures on employers and others. This will drive innovative approaches for absorbing these costs, which can exceed multi-million-dollar price tags for payers and individual patients. Unique financial solutions, such as loan-based programs for payers, significantly offset the cost of expensive and potentially curative CGTs.”
OCTOBER 2023 23
“A shift toward Value-Based (VB) and Outcome-Based contracts promote greater patient access to new biopharmaceutical treatments by linking reimbursement, coverage or payment to a treatment’s realworld performance and patient outcomes,”
says
Specialty Pharmaceuticals
Dea Belazi
Corey Belken
He asserts that another issue will be the evolving role of specialty pharmacies in the management of the specialty medications for the medical benefit, adding, “Payers have typically managed specialty medications on the pharmacy benefit and medical benefit separately, making it challenging to see the full effect of their specialty strategies and where there may be opportunities to improve the patient experience and health outcomes. Specialty pharmacies have the opportunity to manage these benefits seamlessly and assist both the patient and payer in enhancing the quality and cost of the specialty drug therapy regardless of the benefit.”
Belazi points out that specialty pharmacies have the additional opportunity to direct patient care and specialty drug administration sites of care.
“Hospitals typically charge more for specialty drugs and their administration than independent administration sites and physician offices, whether treatment occurs in a hospital or a hospital-owned physician practice,” he explains. “Administering drugs in physician offices and patients’ homes -- instead of hospital outpatient settings -- can significantly reduce costs and provide savings opportunities for both the payer and patient. This approach helps to eliminate hospital stays, decreases hospital utilization, hospital resources and subsequent cost.”
Finally, he emphasizes that self-funded employers, plan sponsors and other payers are contracting directly with an SP provider in designing their benefit packages.
“This enables payers to gain better control over SP costs, have greater transparency into their benefit claims and strengthen their negotiating power.”
People

Hiring the best, so our clients get the best
Partnerships
Partnerships that move us all into a brighter future


Programs
New programs and concierge services for improved outcomes and savings

Technology
A world-class experience with next-generation technology
Brand Brick & Mortar

Maintaining a fresh brand and space to reflect who we are
Better outcomes, savings and solutions for a better tomorrow.
HPI is a proud sponsor of the SIIA23 – Connect National Conference
Connect
We can’t wait to see you there.
hpiTPA.com
24 THE SELF-INSURER
with us on LinkedIn so we can connect at the conference!
At HPI, we’re investing in the future.
Specialty Pharmaceuticals
Ringmaster is dedicated to developing cloud-based software that will improve your Stop-Loss and PBM administration and the reporting capabilities for Carriers, Managing General Underwriters (MGUs), Third Party Administrators (TPAs), Brokers and PBMs.

By automating the manual processes, you will:
• Reduce processing time and complexity
• Access extensive data warehouse
• Receive real-time actionable analytics
• Minimize turn-around time
330.648.3700 • rmtsales@ringmastertech.com
www.ringmastertech.com Step Into the Ring and Start Realizing the Possibilities by Utilizing Ringmaster’s Cloud-Based Solutions to Make Your Business Thrive!
to one destination to connect partners across the entire PBM & Stop-Loss ecosystem. Start Realizing the Possibilities!
•
Come
All panelists cite the emerging role of value-based or outcomes-based contracting as a topic for discussion. Value-based contracts, sometimes called risk-sharing agreements, are innovative payment models used by payers and biopharmaceutical innovators to link reimbursement, coverage, or payment to a treatment’s real-world performance.
In an outcomes-based contract, payment is wholly or partly dependent on outcomes being achieved. Service providers are therefore directly incentivized to deliver outcomes with service users.
Additionally, they anticipate that employers will be forced to address the new, popular weight loss drugs, as many cut off or restrict access as a way to save money. These cuts and restrictions signal the financial downside of the drugs’ medical success, but people are taking them as a first step to losing significant weight.

Employers that are covering the costs may not be able to afford them. At $1350.00 or more as the monthly cost, employers are having to grapple with the expense despite the fact that their employees are anxious to take these medicines.
They also anticipate a discussion involving greater reliance on copay assistance programs and alternative funding. Copay cards are intended to reduce the total out-of-pocket expense for the patient who may be under-insured and unable to afford the expense. The benefits payer pays some of the cost and then the manufacturer pays part or all of the cost that the patient is responsible for through copay or coinsurance.
Panelists also foresee an important role for Foundations that are established to help offset these costs, including CancerCare, HealthWell Foundation, Leukemia & Lymphoma Society, National Organization For Rare Disorders (NORD) and others.
These resources are helping people to overcome financial access and treatment barriers by assisting them with co-payments for their prescribed treatments. Many offer easy-to-access, same-day approval over the phone and online.
An additional topic which is making headlines will focus on prior authorizations (PA), sometimes referred to as a “pre-authorization.” This is a requirement from the payer that the doctor obtain approval from the plan before it will cover the costs of a specific medicine, medical device or procedure. Most recently, the insurance carrier Cigna announced it would be removing close to 25% of medical services from PA requirements – although not specifically drugs.
In fact, a letter to CMS was recently issued by the American Hospital Association, the American Medical Association, the Blue Cross Blue Shield Association and America’s Health Insurance Plans which united to make the case against proposed prior authorization standards. The groups stated that the provisions of the December 2022 Notice of Proposed Rule Making would create two sets of standards that would slow implementation and add unnecessary costs. The extent to which self-insured employers follow this trend is to be determined.
Dr. Motheral foresees challenges with the emergence of biosimilars, simply defined as a biological medicine highly similar to another already approved biological medicine, referred to as the ‘reference medicine’. Biosimilars are approved according to the same standards of pharmaceutical quality, safety
26 THE SELF-INSURER
Specialty Pharmaceuticals
Dr. Brenda Motheral
and efficacy that apply to all biological medicines.

She highlights the entry of several biosimilars to the Humira brand and questions whether this preferred status of the biosimilar should extend beyond Humira to other drugs in the class. The drug suppresses the immune system by blocking the activity of TNF: a protein produced naturally by the body’s immune system. Some people with certain autoimmune diseases produce too much TNF. Humira is designed to stop tumor necrosis factor-a, or TNF, from attacking healthy cells.
She also forecasts that managing the extremely high cost of cell and gene therapies will require employers to have well defined strategies for addressing these expenses. By the end of 2022, 13 cell and gene therapies were on the US market. In 2023, expectations are that up to 12 new cell and gene therapies will be approved in the US.
OCTOBER 2023 27
“The best-selling drug Humira (adalimumab) now faces competition in the United States after a 20-year monopoly,” says Dr. Motheral. “Eight different biosimilars have launched this year with discounts as large as 85% from Humira’s list price of $6922. A few companies also offer two price points.”
Meritain Health is an independent subsidiary of Aetna and CVS, and one of the nation’s largest employee bene�ts administrators.1 We are uniquely positioned to enable our customers to combine our �exible plan administration, products and external point solutions with the right resources from parent companies Aetna and CVS. 1. Business Insurance; Largest Employee Bene�t TPAs (as ranked by 2019 bene�ts claims revenue); May 2020. Follow us: Simple. Transparent. Versatile.
Meritain Health®, our goal is simple—take a creative approach to health care and build industry-leading connections. Whether you're building an employee bene�ts program, researching your member bene�ts or o�ering support to your patients, we're ready to help you do more with your health plan.
more at www.meritain.com. Specialty Pharmaceuticals
At
Learn

“These treatments typically range from $250,000 to $3.5 million per individual,” she explains. “While these novel therapies serve only small patient populations, employers may be forced to contend with extreme and, in some cases, unsustainable drug costs. With increased pharmaceutical company investment in regenerative medicine and growing interest in rare disease, it is likely that more companies will face these expenditures for these potentially lifesaving treatments.”
Dr. Motheral also believes there will be increased focus upon the best practices for managing specialty drugs under the medical benefit, where many of the gene therapies are covered.
Specialty drugs can be covered insurance based on type of administration, and an estimated 30-50% of specialty drugs are covered under medical benefits, being administered in outpatient facilities, physician offices, or outpatient/ambulatory infusion centers.

She explains that drugs covered under pharmacy benefits are most often self-administered, such as oral medications, self-injectables, or medicines delivered via other methods that patients can manage at home. Drugs that must be administered by a health care provider, which includes many cancer medications, are typically covered by medical benefits.
“There can also be key differences in coverage, depending on whether the drugs are paid for under the medical benefits or pharmacy benefit,” she adds. “The member copays, formularies, and clinical prior authorization programs can vary significantly across the two benefits, resulting in benefit shopping and suboptimal sites of care.”
COSTS CONTINUE TO RISE
The specialty drug trend continues to be driven primarily by claim utilization, accounting for nearly three-quarters of the overall 14.1% gross trend, according to the Walmart report.
It appears that the cost per claim plays a larger role in specialty trend, with the number of members taking specialty drugs continuing to rise: 4% of members took at least one specialty drug in 2022, while the average number of claims per person remained steady. On the surface, this increase may appear minimal, but even a slight increase in the percentage of members taking specialty drugs can have substantial cost implications on a per member per year basis.
The top categories for specialty drug spend show that inflammatory, oncology and multiple sclerosis lead the way, with about 13 oncology drugs approved each year. In 2023, there are 16 oral drugs and 6
Specialty
Pharmaceuticals
On average, aequum r esolves c laims within 297 days of p lacement aequum has generated a savings of 95.5% off disputed c harges f or self-funded pl ans aequum ha s ha ndled claims in all 50 states 297 95.5% 50 No Guarantee of
–
Results
Outcomes depend upon many factors and no attorney can guarantee a particular outcome or similar positive result in any particular case.
1111 Su perior A venue E ast Suite 1360 Cleveland, OH 44114 P 2 16-539-9370 www.aequumhealth. com OCTOBER 2023 29
Protecting plans and patients across the U.S.

Partner with Nationwide® to simplify Medical Stop Loss for you and your clients. Save time and effort with easy access to experienced underwriters who offer a broad range of solutions. Our flexible plans are tailored to fit your clients’ needs and reduce future risk. Plus, claims are backed by a carrier with A+ financial ratings.* Offer coverage from a brand clients can trust. Nationwide has been in the health business for 80 years and Medical Stop Loss for nearly 20 years. To learn why top Medical Stop Loss producers and underwriters choose Nationwide, call 1-888-674-0385 or email stoploss@nationwide.com We hope to see you at the SIIA National Conference. *A+ ranking from AM Best received 10/17/02, affirmed 12/1/22, and A+ ranking from Standard & Poor’s received 12/22/08, affirmed 4/19/22. Plans are underwritten by Nationwide Life Insurance Company, Columbus, Ohio 43215. Nationwide, the Nationwide N and Eagle, and Nationwide is on your side are service marks of Nationwide Mutual Insurance Company. © 2023 Nationwide NSV-0113AO.1 (06/23) Strong relationships. More solutions.
drugs delivered via injection in the pipeline, with 6 drugs in the pipeline for breast cancer and 3 for non-small cell lung cancer (NSCLC).
These findings suggest that the overall increase in spend is now being driven by the introduction of new specialty utilizers rather than by increased claims among those who already take a specialty drug. Biosimilars also have a profound impact on the overall specialty spend, with biosimilar utilization increasing from 20.5% in 2021 to 26.3% in 2022.
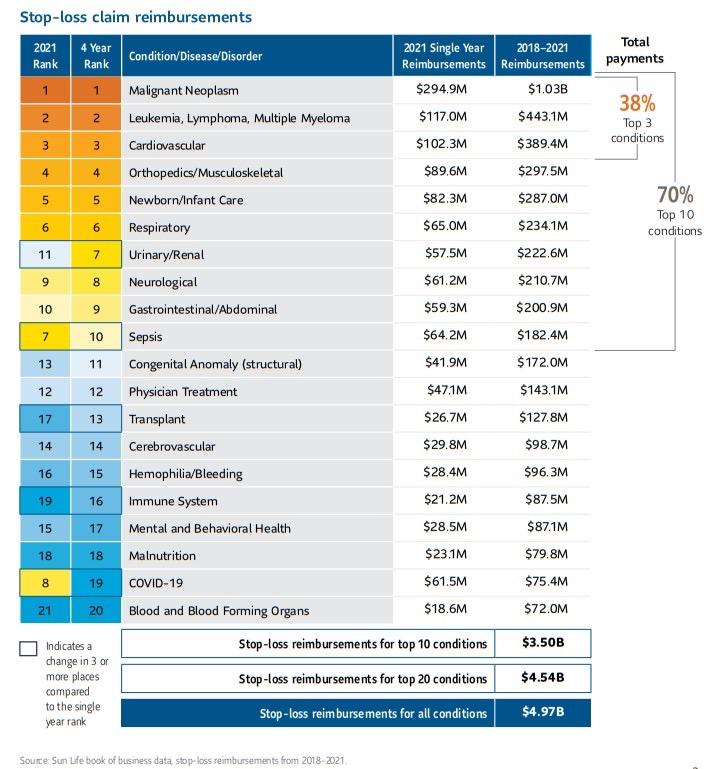

Source: 2023 SunLife
SPECIALTY DRUGS TO WATCH
The latest Sun Life Report reveals that cancer categories Malignant Neoplasm and Leukemia, Lymphoma and Multiple Myeloma continue to be top drivers of highcost claims, making up 29% of total claim reimbursements over the past four years, with cancer drugs comprising over half of the top 20 high-cost injectable drugs for 2022.
The trend report also states that some of the specific drugs have changed:
• Herceptin and Tecentriq have completely dropped out of the top 20.
• Almita, which is used to treat malignant mesothelioma and other lung cancers, moved up two rungs, at an average cost close to $67,000.
• Leukemia and lymphoma drug Rylaze, at an average cost of over $800,000, make it the most expensive drug in the top 20.
OCTOBER 2023 31 Specialty Pharmaceuticals
RISING COSTS AHEAD
The outlook for escalating costs is clear: venerable analysts at PwC’s Health Research Institute anticipate persistent double-digit pharmacy trends driven by specialty drugs and the increasing use of certain medications used to treat Type 2 Diabetes or weight loss.
In a survey they conducted with US health plans, covering 100 million employer-sponsored large and small group members and 10 million Affordable Care Act (ACA) marketplace members, they report that plans are experiencing inflationary pressure from rising median prices of new drugs as well as increasing prices of existing drugs.
Combine with the accelerated approvals of new CGTs, they don’t expect pharmacy trends to slow down in 2024 with the inflationary impact predicted to be in the high single or double digits from 20232024.
They do foresee two “deflators”:
• The adoption and potential of biosimilars to manage these rising drug costs. With the prices of biosimilars on average more than 50% lower than the reference products for which they can substitute, there is substantial opportunity to manage costs. 65% of health plans surveyed ranked biosimilars coming to market among their top cost deflator.

• Site of care is shifting from expensive hospital settings to less expensive sites, such as independent administration sites, physician offices and patients’ homes. In fact, one report said that close to two-thirds of Immune Checkpoint Inhibitors (ICI) also known as immunology treatments are administered by outpatient clinics at hospitals, where it costs $157,000 each year on average to receive care. By comparison, it costs $87,000 on average annually for a patient to receive the infusions in a doctor’s office.
Additional reports, such as one survey released from the Pharmaceutical Strategies Group, raises concerns about the lack of uptake in value-based or outcomes-based contracting for specialty drugs.
They polled more than 180 employers, insurers and labor unions and found that just 12% are using value-based models for pricey specialty therapies, with payers citing multiple hurdles to rolling out these models.
Payers are demanding to see more evidence that the models are effective and can’t seem to agree on methodologies for tracking outcomes.
32 THE SELF-INSURER
Specialty Pharmaceuticals
What is encouraging is that the survey also found that 14% of employers and 7% of health plans are deploying alternative funding models, while 14% and 33%, respectively, are exploring their use – although a majority of those polled said they don’t view these models as sustainable.
While co-pay assistance programs drew positive responses that they are necessary to assist people in affording high-cost medications, there was some respondents who said that at these programs encourage patients to take pricier brand-name drugs rather than select the lower-cost alternative medication.

It appears from this survey that the primary concern in this space is ensuring parity in costs across both the medical benefit and pharmacy benefit. Employers remain challenged on the issue of affordability and cost-sharing for members, with the majority of surveyed payers using PA for these drugs while expressing concerns about the potential for unintended related consequences, such as member dissatisfaction or care delays.
Clearly, these topics and findings reflect and complement the topics that are addressed at the SIIA panel presentation. What is so compelling is that employers will find the panelists’ guidance and recommended strategies highly valuable in the year ahead.
Laura Carabello holds a degree in Journalism from the Newhouse School of Communications at Syracuse University, is a recognized expert in medical travel, and is a widely published writer on healthcare issues. She is a Principal at CPR Strategic Marketing Communications. www.cpronline.com
Sources:
Report: Specialty drug trend, costs will continue to rise | Drug Store News
https://drugstorenews.com/report-specialty-drug-trend-costs-willcontinue-rise
https://www.benefitspro.com/2023/07/11/the-10-highest-cost-claimconditions-for-2022/
https://www.pwc.com/us/en/industries/health-industries/library/ behind-the-numbers.html
https://www.fiercehealthcare.com/payers/survey-why-value-basedcontracting-specialty-drugs-remains-rare
https://www.healthcarefinancenews.com/news/cigna-remove-25medical-services-prior-authorization#:~:text=The%20company%20 has%20now%20removed,1%2C100%20medical%20services%20 since%202020.&text=Cigna%20Healthcare%2C%20the%20health%20 benefits,requirements%2C%20the%20insurer%20said%20today.
OCTOBER 2023 33 Specialty Pharmaceuticals
We Know ... Risk
We study it, research it, speak on it, share insights on it and pioneer new ways to manage it. With underwriters who have many years of experience as well as deep specialty and technical expertise, we’re proud to be known as experts in understanding risk. We continually search for fresh approaches, respond proactively to market changes, and bring new flexibility to our products. Our clients have been benefiting from our expertise for over 45 years. To be prepared for what tomorrow brings, contact us for all your medical stop loss and organ transplant needs.


Visit us online at tmhcc.com/life Tokio Marine HCC - Stop Loss Group A member of the Tokio Marine HCC Group of Companies TMHCC1189 - 09/2023 HCC Life Insurance Company operating as Tokio Marine HCC - Stop Loss Group
COSTLY WEATHER EVENTS FUEL CAPTIVE INTEREST
R
Record
Written By Caroline McDonald
weather events, ranging from flooding and hurricanes to high temperatures and wildfires, have put pressure on insurance companies. These events have led to increasing numbers of claims and costs, with several insurers exiting the property and insurance market in a growing number of states.

This has also given organizations pause to look at alternatives to their property coverage and to plan accordingly.
To secure ongoing coverage, as well as have more control over pricing, organizations are increasingly looking to self-insurance and captives.
OCTOBER 2023 35
WEATHER EVENTS LEAD TO INSURER WITHDRAWALS

Recently Farmers Insurance stopped offering new auto, home and umbrella policies in Florida, citing the growing costs of natural disasters and construction.
In California, AIG, Allstate, State Farm and Farmers have all ceased writing new policies due to weather events, inflation, and reconstruction costs.
AAA has also dropped some coverage in Florida, California, and Louisiana, citing weather risks.
According to McKinsey & Company’s report, “Climate Change and P&C Insurance and Opportunity”:
“The projected escalation of climate risk, such as the occurrence of more floods and wildfires, may lead to underinsurance—or to no insurance at all. The result, substantial market dislocation will include premium loss, higher rates of self-insurance, and an increased demand for disaster relief from the public sector.”
Dale Porfilio, chief Insurance Officer with the Insurance Information Institute, and president of the Insurance Research Council notes
that the nature of insurance is “the balance of availability and affordability. Based on the information they have, if insurers don’t perceive they can achieve a reasonable return on a particular type of risk, they either need to increase the price, or to write less of it,” he said. “With what’s happening now with climate risk, there is a need to be taking prices up.”
In the property market, “From the beginning of the pandemic to the end of 2022, replacement cost prices on losses went up a cumulative 55 percent for homeowners’ writers,” Porfilio said. This means higher costs to repair or replace damaged homes and business.
36 THE SELF-INSURER
The Insurance Regulator State of Climate Risks Survey, conducted by the Deloitte Center for Financial Services, found that:
• A majority of U.S. state insurance regulators expect all types of insurance companies’ climate change risks to increase over the medium to long term—including physical risks, liability risks, and transition risks.
• More than half of the regulators surveyed also indicated that climate change was likely to have a high impact or an extremely high impact on coverage availability and underwriting assumptions.
Shared Values
Hurricanes in Florida and wildfires in California have meant that insurers are having to file for rates as they are able, Porfilio said. Those that are not able to get the rate they need, “are
The extra layer, he said, is that most companies writing property insurance also purchase reinsurance for their book of business. “In part because of Hurricane Ian coming through and the perception of increased climate risk, reinsurance pricing also went up,” Porfilio said.
Higher reinsurance costs means that insurers ultimately have to pass that cost onto consumers, “and that is where it is affecting both personal lines and commercial,” he said.

Customer Service, Cost Controls, Quality Performance
We deliver value other TPAs can’t match. Our three-year medical trend is beating the industry at 1.3% and our claims reviews are finding an extra 15%in savings before network discounts. Our people are working hard to deliver incredible value for our customers. They can do it for you too.
scaling back the amount of business they can write—whether it’s scaling back new business, opening the door for new business or deciding to leave the market—and different companies are making different choices.”
37 OCTOBER 2023 R450-2880
400 Field Drive • Lake Forest, IL 60045 | 800.832.3332 • TrustmarkHB.com ©2023 Trustmark Health Benefits® Scan the QR code with your smart phone to learn more
Bringing the Power of Consumerism to Healthcare
A first-of-its-kind healthcare SuperApp for self-funded plan sponsors that helps members make better decisions around quality medical care delivery, so everyone wins.
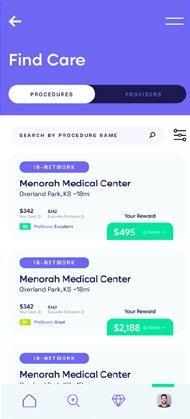
The only self-funded healthcare engagement platform of its kind.
Hercules Health rewards habitual app utilization by giving cash incentives earned through intelligent healthcare shopping tied to quality and cost. More app use equals more savings for members and plan sponsors alike.

Comprehensive Compliance
Hercules Health delivers best-in-class price transparency that is fully compliant with the Transparency in Coverage (TiC) and the No Surprises Act (NSA) rules and regulations.
Contact us today.
herculeshealth.com
info@herculeshealth.com
IMPACT ON COMMERCIAL PROPERTY
While historically there has been greater regulation of personal products than commercial, “Looking at departments of insurance data every quarter, we are seeing commercial property insurance premiums going up more than personal property,” Porfilio said. “This speaks to the fact that if an insurer feels it needs additional premium, they file for it and in general, commercial insurers are able to get higher rate increases than personal property insurers.”
In the commercial property market, “I would say it is all business owners who are affected,” he said. “If you own your own plant, you are the one who has to maintain insurance for that facility. You will have to maintain your own property insurance, and whoever the insurer is, odds are they have purchased reinsurance behind that.” He added, “If you are a renter of an office space or the place where you run your business, your landlord is probably passing that increase to you in the form of higher rent.”
Robert P. Hartwig, clinical associate professor, finance department and director for the Center for Risk and Uncertainty Management at the Darla Moore School of Business, University of South Carolina noted, “Historically, the commercial property insurance markets have been less affected by the factors that are today leading personal
property insurers to freeze, shrink or withdraw from markets such as Florida and California.”

While commercial property insurance rates are not subject to the same degree of rate regulation as the homeowners market, commercial property insurers in Florida, California, and Louisiana, are still vulnerable to the pressures, “associated with the issues driving claim severity: higher inflation, supply chain issues, high labor costs, high catastrophe losses and high reinsurance costs,” he said.
Commercial property insurance markets, “are hard and likely to remain that way for some period of time,” Hartwig said. “Demand for commercial property cover remains strong.”

This demand, in addition to the impetus from the drivers of claim costs, “does give insurers some leverage in terms of pricing,” he said. “Even risks with good loss experience may be seeing doubledigit increases and narrowed terms and conditions upon renewal.”
For these reasons, Hartwig added, commercial property risks could potentially benefit from captive arrangements, “which could allow them to more directly benefit from their own commitment to loss control and risk management.”


While there are potential advantages for commercial property risks using a captive arrangement, captives are “especially attractive for entities

Learn More 8 88-248-8952 selffunding@benefitmall.com ©2023 BenefitMall. All Rights Reserved. Stop-Loss Management Services Claim Risk Solutions Premier Broker Support Expect More FROM YOUR STOP-LOSS PARTNERS 39 OCTOBER 2023
with better-than-average loss performance,” he said.
COVERAGE OPTIONS
If coverage is not available in the private market with standard carriers, “There are three relief valves,” Porfilio said.
1. In some states “you have the Fair Plans—fair access to insurance. This is mostly for personal insurance, but they usually have a commercial insurance component as well. So, you could go to a state run organization like that, and they exist in most states.”
2. Another option is the excess and surplus markets. “Those are outside of the standard regulators. Excess and
surplus means they are operating outside of that and therefore have more latitude on pricing. They generally have more latitude on coverage restrictions, too. So, they may have stripped down some features to make it more affordable, but there is an entire excess and surplus market that operates, on top of the private market,” he said.
3. The third is captives or self-insurance, which “I am hearing is happening more,” he said.

Of these options, he said, “we
Organizations can set up a captive for their property insurance or exclusions. “I met with one of our members that covers personal lines for the high net-worth market,” Porfilio explained. “The finding is that some companies don’t want to write high-valued homes, so companies are placing the liability coverage with standard carriers and are doing combinations of self-insurance or a captive to cover the property risk.”
know the state funds are growing, but we also see that excess and surplus and the captive markets are coming in to fill that void to the extent that they are able.”
40 THE SELF-INSURER
DOMICILES WEIGH IN
Christine Brown, director of captive insurance with the Vermont Department of Financial Regulation noted, “We are definitively seeing growth due to increased rates, unaffordability and unavailability of certain types of coverage and lines of business.”

This has been happening, she said, “in the property space, with interest from large, well established real estate investors and property owners and managers.”
John Huth chairperson of the Montana Captive Insurance Association and an independent captive director, said, “It’s a fairly new phenomenon that companies are pulling out of these states, so I’m sure people are scrambling trying to figure out what to do.”
In the commercial market, he said, captives would be more likely for owners of office buildings and apartment complexes.
A captive, “could be an option for hotel chains with locations in different geographic regions. Or possibly hospitals,” Huth said. “Feasibility studies would have to be considered. You definitely would need a good premium base to even consider a captive.”
Group captives might be more viable for commercial captives with varied types of businesses and locations, he noted. “A group captive is something they could look at, but you would want to diversify your locations. Because if you have a natural disaster that takes out everybody, you’re not going to survive that,” Huth said.
41 OCTOBER 2023
Caroline McDonald is an award-winning journalist who has reported on a wide variety of insurance topics. Her beat has included in-depth coverage of risk management and captives.
“Fatima

“I've


Learn more at Claim-doc.com or call (888) 330-7295 With ClaimDOC you’re in the driver’s seat to create a rich and sustainable healthcare plan using RBP principles. Our approach to elevate the member experience, while diligently managing risk is what sets us apart. Nobody delivers like we do. ClaimDOC’s reference based pricing program is unlike any other. Experience savings and a caring team who is always there to go above and beyond for members.
can’t tell you enough how pleased we are with getting all of our physicians on board.”
“I
was knowledgeable, quickly calmed me down, and put my fears to rest.”
never had such a good customer service experience in my lifetime!”
NAVIGATING COVERAGE FOR WEIGHT LOSS MEDICATIONS
 Written By Kevin Brady, Esq., Director, Plan Document Compliance of The Phia Group
Written By Kevin Brady, Esq., Director, Plan Document Compliance of The Phia Group
I In October of 2022, Elon Musk (one of the world’s wealthiest individuals) ignited headlines when he revealed that he used Wegovy as a primary method for losing weight.
Wegovy, and other drugs such as Ozempic and Mounjaro, instantly became national news and an intriguing weight loss option for people across the country.
By all accounts, these drugs seem to show effectiveness in addressing weight loss concerns; however, it’s important to note that they come with a significant cost.
Specifically, Wegovy, Ozempic, and Mounjaro boast per-treatment list prices of $1,349, $936, and $1,023, respectively.
43 OCTOBER 2023
This scenario often presents a familiar challenge for self-funded group health plans. Employees may express a desire for specific treatments or services to be covered, but the plan may have an understandable reluctance due to the substantial expenses associated with the treatment. Given this situation, group health plans should take a systematic approach:
1. Assess Whether Coverage is Right for Your Plan: Initially, plan sponsors should thoroughly evaluate whether coverage of weight loss drugs aligns with their overall goals. This entails considering the plan’s overall strategy against the preferences and potential health needs of their members.
2. Cost Containment Strategies: If the decision is made to cover weight loss drugs, plans should explore effective strategies to manage the costs linked to these medications. This might involve proactive conversations with their Pharmacy Benefit Managers (PBM), medical management techniques, or exploring potential alternatives to reduce expenses.
3. Update Plan Documents: To ensure clarity and alignment with revised coverage decisions, plan sponsors should review and update their plan documents accordingly. This includes coverage details and communication to members about the inclusion of weight loss drugs as a covered benefit and any associated medical management techniques.
By methodically addressing these issues, plan sponsors can better navigate the complexities of covering weight loss drugs. This approach promotes informed decision-making, effective cost management, and transparent communication with plan participants.
With a comprehensive understanding of the considerations surrounding the coverage of weight loss drugs such as Wegovy, Ozempic and Mounjaro, let’s now delve into each of the three key aspects in greater detail.
1. ASSESS WHETHER COVERAGE IS RIGHT FOR YOUR PLAN
PROS:
The primary argument in favor of covering weight loss drugs is the potential to improve employees’ overall health. Obesity is closely linked to a range of health problems, including diabetes, heart disease, and joint issues.

By providing access to medications like Ozempic and Wegovy, which are approved by the FDA and have demonstrated effectiveness in aiding weight loss, employers could contribute to reducing these health risks among their workforce. (Wegovy is FDA approved for weight loss while Ozempic is currently only approved for diabetes treatment).
Coverage may also impact employee productivity and morale. Employees may ask about coverage. While this may not be the most important factor in recruiting new employees or retaining current employees, it may give a leg up to employers who offer coverage.
44 THE SELF-INSURER
Furthermore, employees who are healthier are often more productive. By promoting weight loss through covered medications (and other means), employers may see reduced absenteeism due to health-related issues and increased employee engagement. Finally, while these drugs are expensive and require upfront costs, it could lead to longterm savings for employers. Health problems associated with obesity can be expensive to treat, including hospital stays, ongoing medical appointments, and more serious chronic conditions. By investing in weight loss drugs, employers might ultimately mitigate some of these future expenses.
CONS:
The high cost associated with weight loss drugs is the primary argument against coverage. Plan sponsors must evaluate whether the cost of covering these medications aligns with their budget constraints and overall benefits package.

Striking a balance between providing valuable benefits and managing costs is always crucial. As these drugs become more popular, related claim expenses on a group health plan may be significant.
This concern becomes even more significant when considering the necessity for ongoing treatment. To achieve desired results, consistent injections are required. Consequently, discontinuing the drug often leads to weight regain for individuals.
Weight loss drugs, while effective for some individuals, do not guarantee long-term success for everyone. Weight loss is a complex process influenced by various factors including genetics, lifestyle, and mental health.
45 OCTOBER 2023
Granular Insurance is a risk platform to help employers, health care providers, and other stakeholders manage risks, costs, and achieve better outcomes.

Many companies today are looking for ways to combat the increasing volatility of their
Precision Risk approach, Granular Insurance is able to segment risk, reduce variability and deliver a more accurate assessment of a client’s exposure.
What Make’s Granular Unique?
• Precision Risk segments a population into as many as 22 unique cohorts
• with the opportunity for three to ��e�year r�te protection
• Granular clients have access to inno�ati�e tools and ser�ices from Alphabet’s Life Sciences company Verily
A Better Way to Assess Risk
Precision Risk delivers value through more consistent and predictable risk transfer.

75%
10,000 test cases


Shifting Risk from the Employer to Granular

Restructuring Risk
Granular segments a population into as many as 22 unique cohorts, and as a result, can more accurately assess risk, monitor and impact the group’s performance, shift risk from the employer to the carrier and better manage costs.
Underwriting Predictability



Granular deli�ers better estimators and tighter clusters of expected claims costs across the employers’ population, allowing attracti�e rates and multi�year rate and bene�t protection.
Financial Predictability
�ith multi�year rate and bene�t protection, Granular puts ameaningful cap on annual premium increases with moderate and predictable changes to an employers’ spec.
Mind the Gap
Granular offers protection from higher frequency and higher �olatility claims through a mix of speci�c employer stop�loss deductibles, lowering employer risk both at the member le�el and o�erall le�el.
������� � ������������� �� ��������� ���� ������ �or �ore in�or��tion� cont�ct ���e���r�n���rin��r�nce�co�
the employer received more value from Granular’s Precision Risk approach INOF
There is a risk that employees might not experience the desired results, aside from the emotional impact on the individual, this would essentially result in claim expense that does not effectively treat the underlying condition.
Finally, relying solely on medication for weight loss may discourage employees from adopting healthier lifestyle changes. Sustainable weight management often requires a combination of dietary adjustments, regular physical activity, and behavioral modifications. If an individual relies on the weight loss drug to achieve these results, it may have a net-negative effect on their overall health.
2. COST CONTAINMENT STRATEGIES


First, it is imperative to discuss potential options with your PBM. This approach is important to understand the treatment options currently available and whether any generic or lower cost options may be out there.
Next, imposing medical management techniques such as treatment limitations, established medical necessity criteria, and/or prior authorization requirements will limit coverage and the potential claim exposure to the plan.
3. UPDATE PLAN DOCUMENTS
Once the decision to cover weight loss drugs is reached, plan sponsors should update their plan documents to clearly outline the details of this coverage. This includes specifying eligible drugs, criteria for coverage, and any associated costsharing responsibilities for plan participants.
Furthermore, the plan should review the plan document in its entirety to ensure that other language within the plan document does not contradict or otherwise limit coverage on the drugs unintentionally. For example, a general exclusion for “services related to obesity”
PBM Services that Bridge the Gap Between Experience & Technology
Prescription spending is rising with no end in sight, but ELMCRx Solutions is the PBM services company that gets the full picture. Discover how much our cutting-edge tech platform and expert team of pharmacists can save plan sponsors.

For more information, contact Mary Ann Carlisle: 484.433.1412 | mcarlisle@elmcgroup.com elmcrx.com Specialty and High-Cost Drug Management Clinical Case Management Non-Specialty Drug Management Prior Authorization Review Clinically Grounded. Technology Focused. Supported by superior technology and analytics. 47 OCTOBER 2023
should be removed from the document entirely or modified to specify that the exclusion does not apply to these drugs.
Transparent communication with plan participants is essential. Health plans should effectively communicate that coverage is available and provide details on any medical management criteria or techniques that may be relevant for participants. This ensures that members are wellinformed and understand their coverage options.
CONCLUSION
The decision to cover weight loss drugs is a multi-faceted one that is likely unique for each employer.

This decision point will likely be relevant for the foreseeable future. As weight loss drugs continue to make headlines across the country, drug coverage, cost containment strategies, and proper plan language will be essential to ensuring that the plan is protected from increasing claim expense and put into the best possible position to provide meaningful benefits to its participants.
Kevin Brady joined The Phia Group Consulting team as an attorney in the summer of 2019. As the Director of Plan Document Compliance, Kevin works on general consulting, plan document compliance, contract gap reviews, and general compliance issues. While at Michigan State University College of Law, Kevin worked in the MSU College of Law Immigration Clinic. After law school, Kevin worked as an attorney representing several healthcare providers in the Midwest.
48 THE SELF-INSURER
ACA, HIPAA AND FEDERAL HEALTH BENEFIT MANDATES:

PRACTICAL Q & A
Q & A
TheAffordable Care Act (ACA), the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and other federal health benefit mandates (e.g., the Mental Health Parity Act, the Newborns and Mothers Health Protection Act, and the Women’s Health and Cancer Rights Act) dramatically impact the administration of self-insured health plans. This monthly column provides practical answers to administration questions and current guidance on ACA, HIPAA and other federal benefit mandates.
Attorneys John R. Hickman, Ashley Gillihan, Carolyn Smith, Ken Johnson, Amy Heppner, and Laurie Kirkwood provide the answers in this column. Mr. Hickman is partner in charge of the Health Benefits Practice with Alston & Bird, LLP, an Atlanta, New York, Los Angeles, Charlotte, Dallas and Washington, D.C. law firm. Ashley, Carolyn, Ken, Amy, and Laurie are senior members in the Health Benefits Practice. Answers are provided as general guidance on the subjects covered in the question and are not provided as legal advice to the questioner’s situation. Any legal issues should be reviewed by your legal counsel to apply the law to the particular facts of your situation. Readers are encouraged to send questions by E-MAIL to Mr. Hickman at john.hickman@alston.com.
OCTOBER 2023 49
AGENCIES ISSUE EXTENSIVE MHPAEA GUIDANCE: PLAN AND TPA ACTION REQUIRED
On July 25 the Departments of Labor, Treasury, and Health and Human Services issued a proposed rule on requirements related to the Mental Health Parity and Addiction Equity Act (MHPAEA). The Proposed Rule, if finalized in its current form, will impose significant new compliance obligations on group health plans and health insurance issuers and would be effective for plan years beginning on or after January 1, 2025.
The focus on the Proposed Rule is on nonquantitative treatment limitations (NQTLs) under MHPAEA. Along with the Proposed Rule, the departments issued a technical release (TR) related to the Proposed Rule’s data collection requirements, a report to Congress, an enforcement fact sheet, and an MHPAEA guidance compendium.
EXECUTIVE SUMMARY
This Article contains background regarding MHPAEA, a detailed analysis of the Proposed Rule, the TR, and the Report to Congress as well as Practice Pointers but the following is a summary of the key provisions. We will refer to just “group health plans” or “plans” in this Article with the understanding that the MHPAEA requirements are also applicable to health insurance issuers. This article is part 1, with part 2 continuing in the November issue of The Self-Insurer.
NQTLS MUST MEET THREE REQUIREMENTS
Of most significance, the Proposed Rule provides that a plan must satisfy three newly stated requirements to impose NQTLs on mental health and substance use disorder (MH/SUD) benefits.
First, an NQTL that applies to MH/SUD benefits can be no more restrictive than the predominant NQTL that applies to substantially all medical/surgical (Med/Surg) benefits within the same MHPAEA benefit classification.
This “no more restrictive” requirement borrows the mathematical “substantially all/predominant test” that currently exists for financial requirements and quantitative treatment limitations (collectively QTLs) under the 2013 MHPAEA final rule.
Second, the processes, strategies, evidentiary standards, or other factors used in designing and applying the NQTL to MH/SUD benefits must be comparable to (and applied no more stringently than) those
used in designing and applying the NQTL to Med/Surg benefits within the same MHPAEA benefit classification. This requirement codifies the departments’ current view of what must be established in an NQTL comparative analysis.
Third, the Proposed Rule would require the use of outcomes data in analyzing NQTLs. The Proposed Rule would require extensive collection of data, such as claims denials, for an NQTL and then compare data outcomes for both MH/SUD and Med/Surg benefits.
A “material difference” in outcomes represents a “strong indicator” of an NQTL violation, and certain action would need to be taken and documented. While this data collection requirement applies to all NQTLs, there are additional unique data collection requirements for the “network composition” NQTL.
For this NQTL, material differences in the data would go beyond a strong indicator of an MHPAEA violation but would establish that there was an actual violation.
The TR goes into detail regarding the extensive data that plans would need to collect to establish parity/comparability for the network composition NQTL. Based on this outcomes data, the TR notes the possibility of creating a safe harbor for this specific NQTL. The TR asks for comments on that data collection and safe harbor.
50 THE SELF-INSURER
The Proposed Rule does contain important exceptions for “independent professional medical or clinical standards” as well as standards to prevent “fraud, waste, and abuse.” Those exceptions apply to each of these three NQTL requirements.
MEANINGFUL BENEFITS IN EACH MHPAEA BENEFIT CLASSIFICATION
The 2013 MHPAEA final rule provides that if a plan provides MH/SUD benefits in one of the MHPAEA benefit classifications, it must provide MH/SUD benefits in all MHPAEA benefit classifications.
The Proposed Rule would amend and expand this requirement to
require that a plan provide “meaningful benefits” in each classification compared to Med/Surg benefits. The Proposed Rule contains two examples providing clarification of this “meaningful benefits” requirement.
CONTENT OF AN NQTL COMPARATIVE ANALYSIS
The Consolidated Appropriations Act, 2021 (CAA 2021) required each plan to have a written NQTL comparative analysis with five elements: (1) the identification of NQTLs and the MH/SUD and Med/Surg benefits the NQTLs apply to; (2) the factors used to determine application of the NQTLs; (3) the evidentiary standards used to develop the factors; (4) an analysis of processes, strategies, evidentiary standards, and factors demonstrating comparability; and (5) specific findings and conclusions. The Proposed Rule reorganizes and expands on these elements, incorporating a demonstration of the three requirements for NQTLs as part of the comparative analysis.
OTHER PROVISIONS
The Proposed Rule provides further detail on actions the departments may take if they find an NQTL comparative analysis lacking. The departments, for example, can require that the plan eliminate the

51 OCTOBER 2023

You Can. Discover The Value Of Partnership A Full Service MGU Program Manager Custom Plans | EPO | RBP | PPO | Level Funding What If You Could Have The Value Of A Direct Carrier, With The Underwriting Expertise Of An MGU?
NQTL as it applies to MH/SUD benefits. Specific time periods are provided for responding to a department’s initial request for an NQTL comparative analysis and follow-up requests.
For ERISA-covered plans, the Proposed Rule provides that the NQTL comparative analysis is an instrument under which a plan is established or operated under Section 104(b)(4) of ERISA and must be provided to participants and beneficiaries within 30 days of a written request. If not provided, the plan administrator could face up to a $110 per day penalty for not providing that comparative analysis.
Previously, state and local governmental plans could opt out of MHPAEA. The Consolidated Appropriations Act, 2023 ended that opt-out and provided a sunset timetable. The Proposed Rule would implement those sunset provisions.
REPORT TO CONGRESS
In many respects, the departments’ 2023 MHPAEA Comparative Analysis Report to Congress is like the 2022 MHPAEA Report to Congress. Both reports noted that even though plans were required to have a written NQTL comparative analysis by February 10, 2021, many plans were still unprepared to submit their comparative analyses upon request.
Steadfast protection for the unpredictable

And when the comparative analyses were provided, they failed to contain what the departments viewed as required information. The DOL states that it has “not seen a marked improvement in the sufficiency of the initial comparative analyses received” since 2022.
The 2023 report reiterated four NQTLs the DOL is concentrating its enforcement efforts on, as announced in 2021 FAQs. The 2023 report also added two new NQTLs.
Those that were identified in 2022 were (1) prior authorization requirements for in-network and out-of-network inpatient services; (2) concurrent care review for in-network and out-of-network

that weathers any storm
53 OCTOBER 2023
Our Stop Loss Insurance
–
Trust the provider that’s
and
visit voyastoploss.com for more information Stop Loss Insurance is underwritten by ReliaStar Life Insurance Company (Minneapolis, MN) and ReliaStar Life Insurance Company of New York (Woodbury, NY). Within the State of New York, only ReliaStar Life Insurance Company of New York is admitted, and its products issued. Both are members of the Voya® family of companies. Voya Employee Benefits is a division of both companies. Product availability and specific provisions may vary by state. ©2022 Voya Services Company. All rights reserved. 2225973 204657-06012022
Stop Loss coverage
mitigates the impact of devastating medical claims through flexible contracts, customizable plans and a consultative, client-focused approach. With more than 40 years of industry experience, we provide unparalleled guidance and protection for businesses
whether you’re carving out Stop Loss for the first time or an experienced client looking for cost containment.
stopped loss over
over again:
You want unparalleled customer service. Employers need the right stop loss coverage. At Swiss Re Corporate Solutions, we deliver both. We combine cutting-edge risk knowledge with tech-driven solutions and a commitment to put our customers first. We make it easy to do business with us and relentlessly go above and beyond to make stop loss simpler, smarter, faster and better. We’re addressing industry inefficiencies and customer pain points, moving the industry forward – rethinking employer stop loss coverage with you in mind. corporatesolutions.swissre.com/esl
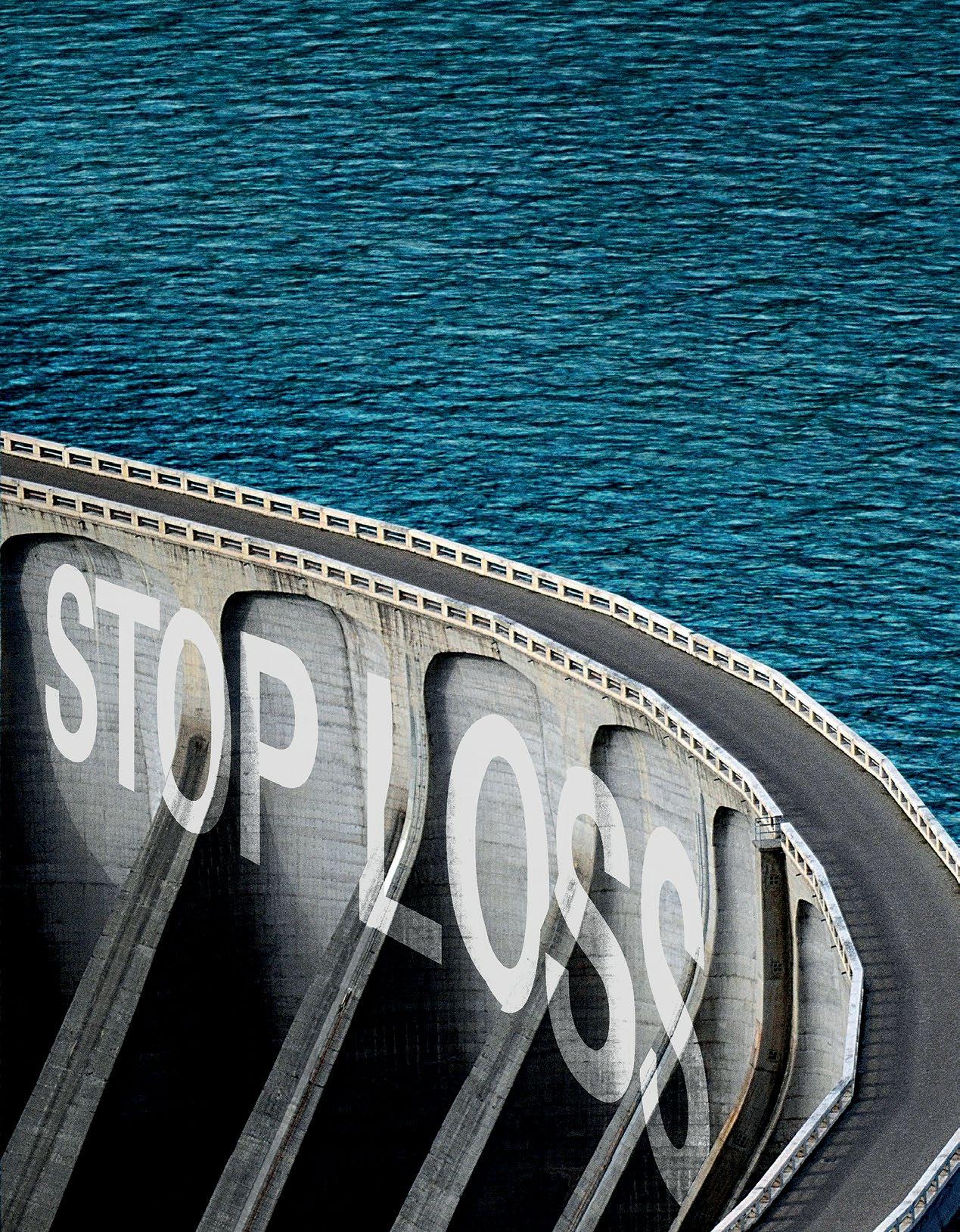
Insurance products underwritten by Swiss Re Corporate Solutions America Insurance Corporation. © Swiss Re 2022. All rights reserved.
Advancing
Together.
Employer Stop Loss: Limit Health Care Exposure.
Self-funding
inpatient and outpatient services;
(3) standards for provider admission to participate in a network, including reimbursement rates; and (4) out-of-network reimbursement rates (methods for determining usual, customary, and reasonable charges).
Added to this list in the 2023 report are (5) impermissible exclusions of key treatments for mental health conditions and substance use disorders; and (6) adequacy standards for MH/SUD provider networks.
The DOL noted its continuing focus on service providers and seeking any plan correction through those service providers. The DOL stated it was expanding its approach by “sending request letters or subpoenas to three more service providers, including some of the largest in the country.”
BACKGROUND
THE LEGISLATION
MHPAEA was enacted on October 3, 2008 and broadly requires that group health plans and health insurance issuers ensure that the financial requirements and treatment limitations that apply to MH/SUD benefits are no more restrictive than those that apply to Med/Surg benefits.
MHPAEA applies to plans sponsored by private and public sector employers with more than 50 employees, including self-funded and fully insured arrangements. The Affordable Care Act, through the requirement to offer “essential health
benefits,” also made MHPAEA apply to small non-grandfathered fully insured plans.
THE 2013 FINAL RULE
A final rule was issued in 2013 that contained separate provisions for QTLs and NQTLs.
QTLs are “quantitative” or numeric aspects of group health plans such as deductibles, copays, co-insurance, maximum out-of-pocket, and visit limits. The QTLs that apply to MH/SUD benefits are required to be no more restrictive than the predominant QTLs that apply to substantially all Med/Surg benefits in a classification. This is referred to as the “substantially all/predominant test.”
The final rule established six benefit classifications. The QTL substantially all/predominant test must be applied to each classification:
• Inpatient, in-network.
• Inpatient, out-of-network.
• Outpatient, in-network.
• Outpatient, out-of-network.
• Emergency care.
• Prescription drugs.
The final rule allowed certain limited subclassifications for drug tiering, in-network tiering, and an outpatient subclassification for office visits.
The Proposed Rule confirms that these classifications and subclassifications apply equally to NQTLs.
Practice Pointer: A group health plan cannot expand this list of classifications and subclassifications. For example, there is no separate classification for telehealth. The Proposed Rule emphasizes this point: “The departments expect plans and issuers to treat telehealth benefits the same way they treat those benefits when provided in person in determining the classification or sub-classification in which a particular benefit belongs.” There are often different QTLs (copays and co-insurance) that apply to telehealth, raising QTL issues, and often the MH/SUD benefits offered through telehealth might be more limited than those offered for Med/Surg benefits, raising NQTL issues.
55 OCTOBER 2023
For QTLs, the final rule defined “substantially all” as two-thirds and “predominant” as more than one-half. If a QTL does not apply to substantially all Med/Surg benefits in a classification, it cannot apply to any MH/SUD benefits in that classification.
For example, if in-network, outpatient Med/Surg services were equally divided between copays and co-insurance (i.e., 50/50), based on claims, then there is no cost-sharing that applied to substantially all (i.e., 2/3) Med/Surg benefits and no cost sharing could then apply to MH/SUD benefits.
If, however, copays applied to substantially all Med/Surg benefits in that classification, then an analysis would look to the predominant copay. If, for example, the Med/Surg in-network primary physician office visit copay was $20 and the specialist copay was $40, then based on plan payments, a determination would need to be made on the predominant copay.
If the predominant copay was $20, then only a $20 copay could be charged for an MH/SUD in-network office visit and the specialist copay could not be charged. The substantially all/predominant test now takes on added meaning since the Proposed Rule adopts this test for NQTLs in a slightly modified fashion.
The final rule set forth parity protections for NQTLs as well. NQTLs are any limitations on the scope or duration of treatment that are not expressed numerically. The final rule and subsequent guidance provided the following illustrative (nonexclusive) list of NQTLs. This list would be slightly modified under the Proposed Rule.
• Plan methods for determining usual, customary, and reasonable charges.
• Refusal to pay for highercost therapies until it can be shown that a lower-cost therapy is not effective (also known as “fail-first” policies or “step therapy” protocols).
• Exclusions of specific treatments for certain conditions.
• Restrictions on applicable provider billing codes.
• Standards for providing access to out-of-network providers.
• Exclusions based on failure to complete a course of treatment.
• Medical management standards limiting or excluding benefits based on medical necessity or medical appropriateness, or based on whether the treatment is experimental or investigative.
• Prior authorization or ongoing authorization requirements.
• Concurrent review standards.
• Formulary design for prescription drugs.
• For plans with multiple network tiers (such as preferred providers and participating providers), network tier design.
• Standards for provider admission to participate in a network, including reimbursement rates.
• Restrictions based on geographic location, facility type, provider specialty, and other criteria that limit the scope or duration of benefits for services provided under the plan.
The final rule provided that a plan may not impose an NQTL on MH/SUD benefits in any classification unless, under the terms of the plan as written and in operation, any processes, strategies, evidentiary standards, or other factors used in applying the NQTL to MH/SUD benefits in a classification are comparable to, and are applied no more
56 THE SELF-INSURER


Health Plan Savings That Stick Full-service RBP solutions. High-touch member support. imagine360.com Your company’s health plan can do better. We promise.
by Quantum Health
Powered
stringently than, the processes, strategies, evidentiary standards, or other factors used in applying the limitation to Med/Surg benefits.
CAA 2021
CAA 2021 was enacted on December 27, 2020 and expressly required group health plans to perform and document a comparative analysis of the design and application of NQTLs. Beginning 45 days after CAA 2021’s enactment (February10, 2021), a group health plan was required make its comparative analysis available upon request from any department.
The comparative analysis must have five different pieces of information as described in the Executive Summary above. FAQs issued in April 2021 clarified these requirements and stated that at a minimum a comparative analysis must have a “robust discussion” of nine different elements.
• A clear description of the specific NQTL, plan terms, and policies at issue.
• Identification of the specific MH/SUD and Med/Surg benefits the NQTL applies to within each benefit classification and a clear statement of which benefits identified are treated as MH/SUD and which are treated as Med/Surg.
• Identification of any factors, evidentiary
standards or sources, or strategies or processes considered in the design or application of the NQTL and in determining which benefits are subject to the NQTL, including any weighting of factors.
• To the extent the plan defines any of the factors, evidentiary standards, strategies, or processes in a quantitative manner, it must include the precise definitions used and any supporting sources.
• An explanation of any variation in the application of a guideline or standard used by the plan between MH/SUD and Med/Surg benefits and a description of the process and factors used for establishing that variation.
• If the application of the NQTL turns on specific decisions in the administration of the benefits, the plan should identify the nature of the decisions, the decision-makers, the timing of the decisions, and the qualifications of the decision-makers.
• If the plan relies on any experts, the analysis should include an assessment of each expert’s qualifications and the extent to which the plan ultimately relied on each expert’s evaluations.
• A reasoned discussion of the plan’s findings and conclusions on the comparability of the processes, strategies, evidentiary standards, factors, and sources identified within each affected classification, and their relative stringency, both as applied and as written. The discussion should include citations to any specific evidence considered and any results of analyses indicating that the plan or coverage is or is not in compliance with MHPAEA.
• The date of the analysis and the name, title, and position of the person or persons who performed or participated in the comparative analysis.
As noted in the 2022 and 2023 reports to Congress, the departments found that every initial comparative analysis reviewed was insufficient.
THE PROPOSED RULE AND TECHNICAL RELEASE
PURPOSE OF THE RULE
The Proposed Rule begins with a new statement of purpose to ensure that:
• MH/SUD “benefits are not subject to more restrictive lifetime or annual dollar limits, financial requirements, or treatment limitations with respect to those benefits than the predominant
58 THE SELF-INSURER
dollar limits, financial requirements, or treatment limitations that are applied to substantially all medical/surgical benefits covered by the plan.”
• Plans “must not design or apply financial requirements and treatment limitations that impose a greater burden on access” to MH/SUD benefits under the plan than they impose on access to generally comparable Med/Surg benefits.
• All statutory and regulatory provisions affecting MHPAEA should be interpreted in a manner consistent with the stated purpose.
Practice Pointer: Although the statement of purpose for the Proposed Rule may appear broad and generic, it evidences the departments’ intent to take a holistic approach to enforcement to make sure that there is actual parity in operation— requiring a plan to establish that it provides participants and beneficiaries appropriate access to MH/SUD benefits.
NEW AND REVISED DEFINITIONS
The Proposed Rule would remove perceived flexibility in defining mental health benefits, medical surgical benefits, and substance use disorder benefits by limiting the effect of any reference to state law and specifically requiring the definition to align with “generally recognized independent standards of current medical practice.”
While plans could still reference state law, they could only do so to the extent state law is consistent with those standards—specifically the most current versions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD).
Practice Pointer: In the past, some plans have tried to classify autism spectrum disorders and eating disorders as a Med/Surg condition rather than an MH/SUD condition. T he preamble to the Proposed Rule notes that since autism and eating disorder are in the DSM as MH/SUD conditions, they must be covered as MH/SUD conditions and cannot be treated as Med/Surg even if state law might provide otherwise.
There are new definitions for “factors,” “processes,” “strategies,” and “evidentiary standards,” which are all currently used in the NQTL comparative analysis. These terms were also used in the 2013 final rule but not defined.
Factors include all information that a group health plan relied on to design an NQTL. The preamble emphasized that “factors” should be read broadly and include all information, including processes and strategies, that were relied on in developing the NQTL. Processes and strategies are then treated as subsets of factors.
Factors would also include information that was considered but rejected. This definition has a nonexhaustive list of factors such as provider discretion in determining a diagnosis or type or length of treatment, clinical efficacy of any proposed treatment or service, licensing and accreditation of providers, claim types with a high percentage of fraud, quality measures, treatment outcomes, severity or chronicity of condition, variability in the cost of an episode of treatment, high cost growth, variability in cost and quality, elasticity of demand, and geographic location.
Processes are actions, steps, or procedures that a group health plan uses to apply an NQTL. Processes can include actions, steps, or procedures established by the plan for a participant or beneficiary to access benefits. For example, processes can include things such as the actual written and operational steps of a preauthorization process or a concurrent review process. They could also include the development and approval of a treatment plan. This definition provides other nonexclusive examples of processes.
59 OCTOBER 2023
Strategies are practices, methods, or internal metrics that a plan considers, reviews, or uses to design an NQTL. Some examples of strategies provided in this definition include the development of the clinical rationale used in approving or denying benefits, deviation from generally accepted standards of care, the selection of information deemed reasonably necessary to make a medical necessity determination, and rationales used in selecting and adopting certain threshold amounts, professional protocols, and fee schedules.
Evidentiary standards are any evidence, sources, or standards that a group health plan considered or relied on in designing or applying a factor in an NQTL. They include specific benchmarks and thresholds. Evidentiary standards may be empirical, statistical, or clinical in nature.
They include items such as recognized medical literature, professional standards and protocols, published research studies, payment rates for items and services (such as publicly available databases of the “usual, customary, and reasonable” rates paid for items and services), clinical treatment guidelines, and internal plan data or criteria for assuring a sufficient mix and number of network providers. The Proposed Rule emphasizes in several places that evidentiary standards are used to develop factors and are not factors themselves.
Practice Pointer: Although the definitions are only in the Proposed Rule, factors, processes, strategies, and evidentiary standards are all key aspects of what the departments currently view as central requirements of an NQTL comparative analysis. Using these definitions as part of a comparative analysis should satisfy the departments that correct definitions are being used.
Planned Administrators, Inc. has been in the industry for more than 40 years and provides a comprehensive experience for all groups, including pharmacy, stop loss, benefit ads ins, and additional perks for members. Contact us today to learn more: paisc.com/contact-us

60 THE SELF-INSURER
Experience More Than Just Benefits Administration
Although not contained in the definitions section of the Proposed Rule, there is a change in wording in the nonexhaustive sample list of NQTLs.
What was previously described as “[s]tandards for provider admission to participate in a network, including reimbursement rates” has been replaced and expanded with “standards related to network composition, including but not limited to, standards for provider and facility admission to participate in a network or for continued network participation, including methods for determining reimbursement rates, credentialing standards, and procedures for ensuring the network includes an adequate number of each category of provider and facility to provide covered services under the plan or coverage.”
The preamble notes that, in the departments’ view, the standards that govern how a network is constructed and defined is a critical NQTL affecting the delivery and availability of MH/ SUD benefits. The Proposed Rule contains specific new provisions for network composition.
THE SUBSTANTIALLY ALL/ PREDOMINANT TEST AS APPLIED TO NQTLS
As mentioned in the Executive Summary, for NQTLs the Proposed Rule would apply the substantially/all predominant test that currently applies to QTLs. If finalized, this test might dramatically affect plan design.
The previous understanding of the 2013 final rule was that a plan could have a NQTL, such as prior authorization, that applies to some but not all MH/SUD benefits and applies to some but not all Med/Surg benefits.
Then, if the factors, processes, strategies, and evidentiary standards in developing and applying the NQTL were comparable for MH/SUD and Med/Surg benefits, there was no MHPAEA violation even if the NQTL applied to more MH/SUD than Med/Surg benefits.
There is an example of this concept in the final rule. That example is deleted in the Proposed Rule and replaced by one incorporating the substantially all/predominant test and the proposed required analysis of data outcomes.
The first part of this test is that any NQTL that applies to MH/SUD benefits in a classification must apply to substantially all Med/Surg benefits in that classification. “Substantially all” is defined as twothirds.
While the Proposed Rule gives several examples of the “predominant” requirement of this test, it does not provide an example solely dedicated to just the substantially all part of the test. But looking at the actual Proposed Rule itself, it could affect NQTLs such as preauthorization especially for outpatient benefits (whether in network or out of network).
If the preauthorization requirement does not apply to at least twothirds of the Med/Surg benefits in the applicable classification, then it cannot be imposed on MH/SUD benefits in that classification.
Practice Pointer: Intensive outpatient treatment and partial hospitalization are usually treated as outpatient benefits for MH/SUD purposes. Those treatments are often subject to preauthorization. Under the Proposed Rule, preauthorization could not be required for these benefits in an outpatient, innetwork classification unless preauthorization was required for two-thirds of Med/Surg benefits in that classification. We believe that many plans will have difficulty meeting this threshold. Under the Proposed Rule, all outpatient NQTLs will need to be examined closely. There are, however, important exceptions for “independent professional medical or clinical standards,” as well as standards to prevent “fraud, waste, and abuse.”
The substantially all determination is made based on the dollar amounts expected to be paid for Med/Surg benefits in the particular classification for the plan year. Any reasonable method may be used. In the preamble, the departments make several observations on this testing.
61 OCTOBER 2023
Lean
Whether

on
to be your crutch.
us—we want
compliant
it’s
platform
data,
Payor Solutions
industry-leading platforms
TPA, ASO, or network. We Have the Best Standalone Solutions. IntegratedPayorSolutions.com
it’s a transparency tool to keep you NSA
or
an administrative
to automate your
Integrated
has the
to power your
They refer to the rules on QTL testing and the credibility of data with distinctions made between self-funded, large group market, and small group market plans.



They state that in making any projections plans should “document the assumptions used in choosing a data set and making projections.” Similar to QTL testing, they indicated that testing is not required each plan year “unless there is a change in plan benefit design or utilization that would affect an NQTL within a classification.”
The departments acknowledge that the substantially all/ predominant test does not
always fit neatly into an NQTL context and ask for further comments, including on whether there are systems in place to perform this testing.
If the substantially all part of the test is met, then a plan may still only apply the predominant Med/Surg form of the NQTL. The Proposed Rule defines “predominant” as “the most common or frequent variation of the NQTL” (this is slightly different than the “more than one-half” standard for “predominant” in QTL testing).
There is also no definition of what constitutes a variation of an NQTL. As with the substantially all part of the test, which variation of the NQTL is predominant is also based on projected plan payments.
The Proposed Rule does provide two examples. The first is a preauthorization requirement that applies to all inpatient, in-network benefits—both MH/SUD and Med/Surg. Med/Surg benefits are approved for periods of one, three, and seven days, after which a treatment plan must be submitted.
63 OCTOBER 2023
Based on projected plan payments, preauthorization for seven days is the most common duration. For MH/SUD, preauthorization is most commonly given for only one day. In this example, the departments find an MHPAEA violation.
The plan satisfies the substantially all requirement since preauthorization is required for every benefit in the inpatient, innetwork classification. The plan, however, fails the predominant test because the most common approval for MH/SUD is one day instead of the predominant seven days for Med/Surg.
This example does assume that the difference in duration is not the result of independent professional medical or clinical standards or standards to detect or prevent and prove fraud, waste, and abuse.

In another example, concurrent review is required for every inpatient, in-network facility stay. In each instance there is a first-level concurrent review, and if the first-level reviewer is unable to make a medical necessity determination to allow a continued stay, it is escalated to a second-level review.
At this second level, the plan, in operation, conducts a peer-to-peer review for MH/SUD benefits while not requiring a peer-to-peer for Med/Surg. Here again, the concurrent review requirement applies to all benefits in the specific category so the substantially all test is satisfied. The predominant variation of the concurrent review NQTL at the second level of review for Med/Surg is not to apply a peer-to-peer requirement.
Accordingly, the departments conclude the peer-to-peer requirement in operation for MH/SUD benefits at the second level would be an MHPAEA violation. Once again, the example assumes that the application of peer-to-peer for MH/SUD is not the result of any
impartially applied independent professional medical or clinical standards or standards to detect or prevent and prove fraud, waste, and abuse.
Practice Pointer: Distinctions between NQTLs for purposes of the substantially all part of the test and variations in NQTLs for the predominant part of the test may be difficult. It is unclear when a variation in an NQTL becomes so significant that it is actually a separate NQTL.
Part 2 of this article will continue in the November issue of The Self-Insurer.
64 THE SELF-INSURER
NEWS FROM SIIA MEMBERS
OCTOBER 2023 MEMBER NEWS

SIIA Diamond, Gold, and Silver member companies are leaders in the self-insurance/captive insurance marketplace. Provided below are news highlights from these upgraded members. News items should be submitted to membernews@siia.org.
All submissions are subject to editing for brevity. Information about upgraded memberships can be accessed online at www.siia.org.
If you would like to learn more about the benefits of SIIA’s premium memberships, please contact Jennifer Ivy at jivy@siia.org.
66 THE SELF-INSURER
NEWS

DIAMOND MEMBERS
VĀLENZ® HEALTH RANKS NO. 3646 AMONG AMERICA’S FASTESTGROWING PRIVATE COMPANIES

PHOENIX, AZ — Inc. revealed that Vālenz® Health ranked again as one of the fastest-growing private companies in America: No. 3646 on the 2023 Inc. 5000, and No. 215 among health services companies. The prestigious ranking provides a data-driven look at the most successful companies within the economy’s most dynamic segment. Facebook, Chobani, Under Armour, Microsoft, Patagonia and many other brands first gained national exposure as Inc. 5000 honorees before becoming household names over the years.
“It’s truly an honor to be recognized again as one of America’s fastest-growing private companies, and it reinforces the culture that drives our core promise to deliver smarter, better, faster healthcare,” said Rob Gelb, Chief Executive Officer of Valenz. “By reimagining a transparent, data-rich approach to simplifying the complexity of selfinsurance for employers, we deliver the measurable care management,
network innovations and early engagement for improved health outcomes and significant savings, facilitating growth for our company and for our customers.”

Valenz joined the Inc. 5000 list for the first time in 2020 and has continued to experience consistent growth since then. The Inc. 5000 class of 2023 represents companies that have driven rapid revenue growth while navigating inflationary pressure, the rising costs of capital, and seemingly intractable hiring challenges.
Among this year’s top 500 companies, the average median three-year revenue growth rate
68 THE SELF-INSURER NEWS STOP LOSS | CAPTIVE | PAYOR | PROVIDER | GROUP ACCIDENT We love what we do and it shows in the relationships we cultivate with peers, partners and clients. Our stellar reputation is based on trust, expertise and an unparalleled team with eyes on innovation and collaboration. Reach out today and see how we can apply that thinking for you. starlinegroup.com | (508) 809-3179
Depend on Sun Life to help you manage risk and help your employees live healthier lives

By supporting people in the moments that matter, we can improve health outcomes and help employers manage costs.
For over 40 years, self-funded employers have trusted Sun Life to help them manage financial risk. But we know that behind every claim is a person facing a health challenge and we are ready to do more to help people navigate complicated healthcare decisions and achieve better health outcomes. Sun Life now offers care navigation and health advocacy services through Health Navigator, to help your employees and their families get the right care at the right time – and help you save money. Let us support you with innovative health and risk solutions for your business. It is time to rethink what you expect from your stop-loss partner.
Ask your Sun Life Stop-Loss Specialist about what is new at Sun Life.
The content on this page is not approved for use in New Mexico. For current financial ratings of underwriting companies by independent rating agencies, visit our corporate website at www.sunlife.com. For more information about Sun Life products, visit www.sunlife.com/us. Stop-Loss policies are underwritten by Sun Life Assurance Company of Canada (Wellesley Hills, MA) in all states except New York, under Policy Form Series 07-SL REV 7-12. In New York, Stop-Loss policies are underwritten by Sun Life and Health Insurance Company (U.S.) (Lansing, MI) under Policy Form Series 07-NYSL REV 7-12. Product offerings may not be available in all states and may vary depending on state laws and regulations. © 2023 Sun Life Assurance Company of Canada, Wellesley Hills, MA 02481. All rights reserved. Sun Life and the globe symbol are trademarks of Sun Life Assurance Company of Canada. Visit us at www.sunlife.com/us. BRAD-6503-y SLPC 29427 01/22 (exp. 01/24)
ticked up to an astonishing 2,238 percent. In all, this year’s Inc. 5000 companies have added 1,187,266 jobs to the economy over the past three years.
The top 500 companies are featured in the September issue of Inc. magazine, available on newsstands beginning Tuesday, Aug. 23.
“Running a business has only gotten harder since the end of the pandemic,” said Inc. editor-inchief Scott Omelianuk. “To make the Inc. 5000 – with the fast growth that it requires – is truly an accomplishment. Inc. is thrilled to honor the companies that are building our future.”
About Vālenz® Health
Vālenz® Health simplifies the complexities of self-insurance for employers through a steadfast commitment to data transparency and decision enablement powered by its Healthcare Ecosystem Optimization Platform. Offering a strong foundation with deep roots in clinical and member advocacy, alongside decades of expertise in the validation, integrity and accuracy of claims, and a suite of risk affinity solutions, Valenz optimizes healthcare for the provider, payer, plan and member. By leveraging data transparency and delivering an omnichannel approach across the healthcare journey, Valenz improves cost,
quality and outcomes for employers and their members – engaging early and often for smarter, better, faster healthcare. Visit www.valenzhealth. com
About the Inc. 5000 Methodology
Companies on the 2023 Inc. 5000 are ranked according to percentage revenue growth from 2019 to 2022. To qualify, companies must have been founded and generating revenue by March 31, 2019. They must be U.S.-based, privately held, for-profit, and independent—not subsidiaries or divisions of other companies—as of December 31, 2022. (Since then, some on the list may have gone public or been acquired.) The minimum revenue required for 2019 is $100,000; the minimum for 2022 is $2 million. As always, Inc. reserves the right to decline applicants for subjective reasons. Growth rates used to determine company rankings were calculated to four decimal places.
About Inc.
Inc. Business Media is the leading multimedia brand for entrepreneurs. Through its journalism, Inc. aims to inform, educate, and elevate the profile of our community: the risk-takers, the innovators, and the ultra-
CONCERNED ABOUT MEDICAL INFLATION?
WE CAN HELP WITH STARR ESL PREMIERTM: A STOP LOSS INSURANCE PROGRAM FOR EMPLOYERS OF ALL SIZES
Employers are facing unprecedented financial uncertainty in the medical marketplace. Inflation, medical advancements, cutting edge delivery and evolving regulations are all contributing. ESL PremierTM from Starr Insurance Companies can help manage the financial impact in this challenging environment.
TO LEARN MORE CONTACT Mark Duchene mark.duchene@starrcompanies.com 646.466.8485

70 THE SELF-INSURER NEWS

driven go-getters who are creating our future. Inc.’s award-winning work reaches more than 50 million people across a variety of channels, including events, print, digital, video, podcasts, newsletters, and social media. Its proprietary Inc. 5000 list, produced every year since 1982, analyzes company data to rank the fastest-growing privately held businesses in the United States. The recognition that comes with inclusion on this and other prestigious Inc. lists, such as Female Founders and Power Partners, gives the founders of top businesses the opportunity to engage with an exclusive community of their peers, and credibility that helps them drive sales and recruit talent. Visit www.inc. com
SILVER MEMBERS
JEFF FITZGERALD REJOINS STRATEGIC RISK SOLUTIONS
Concord, MA – Strategic Risk Solutions (SRS), the world’s largest independent insurance company manager, announced that Jeff Fitzgerald has rejoined the firm as Managing Director of SRS Benefit Partners, a new division of SRS supporting the establishment and
growth of group and individual Employee Benefit programs.
Mr. Fitzgerald rejoins SRS from Innovative Captive Strategies, where he was Vice President –Employee Benefits. He previously served as Associate Director at Strategic Risk Solutions from 2008-2012.
“We continue to see significant growth in the use of group captives with demand from our partners for enhanced capabilities in development, program support and education. Jeff has extensive experience in working with broker partners in the creation and management of these programs and we are excited to expertise to our existing management and

72 THE SELF-INSURER NEWS LEARN | PLAN | SAVE | PROTECT MULTIPLIED RECOVERY DOLLARS SHIFTED FIDUCIARY DUTY www.phiagroup.com | 781-535-5600 | info@phiagroup.com PERFECTED PLAN DOCUMENTS SECURED LEGAL EXPERTISE
We know what it’s like to feel FOMA, or Fear Of Missing Anything. That’s why we invented Curv®, so you can zero in on catastrophic claims risks with the industry’s most predictive and trusted risk score, making it easier than ever to see more stop loss risks and opportunities—and competitively price plans across your spectrum of underwritten groups.

consulting capabilities,” said Brady Young, SRS CEO.
Mr. Fitzgerald, who has more than 17 years’ experience in group and individual self-funded employee benefits captives, will be based in Charleston, SC.


“SRS is a leader in the captive industry and has been at the forefront in the use of captives for employee benefits,” said Mr. Fitzgerald. “SRS, and its affiliates, have many of the components in place to provide a comprehensive offering to proactively address the challenges of this ever-evolving market. I’m pleased to be
returning to SRS to help expand its presence in the captive market and bring my career back full circle.”
About Strategic Risk Solutions (SRS)
SRS is the world’s largest independent insurance company manager. With 30 years of experience, SRS provides management and consulting services to a wide range of insurance company entities, from single parent captives to complex commercial insurers and reinsurers. SRS has operations in the United States, Canada, Europe, Barbados, Bermuda, Cayman Islands, and South Africa. Visit www.strategicrisks. com
VBA SECURES GROWTH FUNDING WITH $156 MILLION LED BY SPECTRUM EQUITY
Leader in cloud-based benefits software takes on growth partner to meet surging payer demand for next-gen core administrative processing, user engagement and reporting solutions.

YOUR SITUATION IS UNIQUE. YOUR HEALTH PLAN SHOULD BE TOO. Comprehensive self-funded plan management, including medical, dental, vision, COBRA, and reimbursement account administration combined with:
Award-winning support
Experienced, dedicated partnership and guidance
Health plan performance management approach
Optimized costs and health trends
URAC-accredited UM and CM with in-house clinical team Looking for a better way? We’ll help you find it. AskNova@novahealthcare.com novahealthcare.com/services © 2023 Nova Healthcare Administrators, Inc. 74 THE SELF-INSURER NEWS
•
•
•
•
•
Your employer stop loss partner
As a financial leader in the US Health market, we value long-term relationships and work closely with our partners to manage medical risk and limit catastrophic losses. Our team offers a unique customer experience, combing personalized “small town” warmth with “big city” capabilities and expertise.

Discover the advantages of true partnership. www.partnerre.com/health
Milwaukee, WI – VBA, a leader in cloud-based benefits software for healthcare payers, announced that the company has closed a $156 million majority growth equity transaction led by Spectrum Equity, the leading growth equity firm behind healthcare information technology companies Definitive Healthcare and GoodRx. Existing investor Arthur Ventures also participated in the round.

VBA makes the health care experience better for everyone by eliminating data fragmentation and enabling interoperability through its tightly integrated suite of solutions.
VBA serves the entire payer landscape with its next-gen Core Administrative Processing solution (“CAPS”), user engagement platforms, customer support tools, population health reporting solution and robust data connections. The Company’s cloud-based software solutions enable payers to replace outdated legacy systems, grow their business and reduce costs.

“At a time when increasing complexity of plan administration is straining current legacy systems, payers are turning to VBA to help them solve major challenges, from optimizing workflows to responding to customer needs.” said Michael Clayton, President, and CEO of VBA. “We are delighted to bring on Spectrum Equity as a
partner. Their success scaling other healthcare technology and enterprise software companies will be an asset to us as VBA enters its next phase of growth.”
their
“We
NEWS 76 THE SELF-INSURER
Coverage is underwritten by Markel Insurance Company, NAIC # 38970, 10275 West Higgins Road, Suite 750, Rosemont, IL 60018. Terms and conditions for rate and coverage may vary by state and application. Insurance and coverage are subject to availability and qualifications and may not be available in all states. Markel® is a registered trademark of the Markel Corporation. Producer marketing materials. © 2022 Markel Service, Incorporated. All rights reserved. markel.com Imagine the possibilities with Markel® and Nevaeh Markel has developed a strategic collaboration with Nevaeh to provide new product solutions for employer accident and health coverage. Nevaeh products have distinct advantages, but working together provides a leveraging effect that’s called the Nevaeh advantage which includes: • Employer stop loss insurance • Supplemental medical and accident insurance • Outpatient, PBM carve-out plans For more information, visit nevaehinsurance.com
“VBA delivers what payers need today – a smart, efficient way to administer plans with advanced technology,” said Jeff Haywood, Managing Director of Spectrum Equity.
are impressed by
innovative approach and strong customer growth and retention, and we’re eager to leverage our past
A CLEAR PERSPECTIVE STARTS WITH TRANSPARENCY.

The big picture is always in our view – ensuring that you, your business and your members are strong, vigorous and healthy. From our vantage point, that’s possible only when you have open, accessible and accurate information – complete visibility across our Healthcare Ecosystem Optimization Platform.
We transparently share data used to identify cost, network and plan design opportunities, drive claim accuracy, and improve health outcomes for members – keeping a clear perspective on how to make better decisions, together.
That’s our promise to you. This is precisely why our customers stay with Vālenz® Health, because no one else does what we do. For true clarity on achieving smarter, better, faster healthcare, visit valenzhealth.com or call (866) 762-4455.
 Proud to be a Diamond Member
Proud to be a Diamond Member
experience with payer facing tech companies to help them continue to scale.”

“We are excited to back Mike and his team at VBA and accelerate the company’s strategic growth plans” said Michael Radonich, Principal at Spectrum. “Our investment will go towards developing future products and solutions and ensuring the company has the infrastructure and resources needed to support its growing customer base.”
With the investment, VBA will welcome Jeff Haywood and Michael Radonich from Spectrum to the company’s board of directors.
Spectrum Equity was represented by Latham & Watkins LLP. Triple Tree LLC served as Spectrum Equity’s financial advisor.
About VBA Software
VBA is a leading-edge healthcare technology company providing comprehensive software solutions for healthcare payers. Uniquely delivered on a secure, cloud-based platform, VBA provides a suite of technology solutions for core benefits administration. These include CAPS (VBASoftware), user engagement platforms (VBAGateway), customer support tools (VBAVoice), population health reporting solutions (VBAnalytics) and robust data connections (VBAPI). Learn more at www. vbasoftware.com
About Spectrum Equity
Spectrum Equity is a leading growth equity firm providing capital and strategic support to innovative companies in the information economy. Since 1994, the firm has partnered with proven entrepreneurs and management teams to build long-term value in market-leading internet-enabled software and data services companies. Representative investments include Definitive Healthcare, Ease, GoodRx, Origami Risk, Payer Compass, and Verafin. For more information, including a complete list of portfolio investments, visit www.spectrumequity.com
About Arthur Ventures
Arthur Ventures is a Minneapolis-based early growth capital firm that leads investments in B2B software companies. Since 2013, they have partnered with 50+ companies across the United States and Canada. Arthur Ventures manages $1.1 billion and is actively investing out of its $300 million fifth fund. Visit www.arthurventures.com
NEWS 78 THE SELF-INSURER

to efficient Pharmacy Management PharmPix empowers you to take control of your pharmacy benefit and improve the quality of the healthcare you offer to your employees. Be part of the change and come join our team. PharmPix is ready for you! Schedule a demo at www.pharmpix.com or call 404.566.2000
Flexible Accurate Scalable Your path
Don’t face your obstacles alone. Whether you’re facing benefits loading issues, limited reporting, integration problems, or any other challenges—we’ll conquer them by your side.
Rise above your hurdles with cloud-based software fully customized for you.

( Experience quick implementation ( Optimize your software with AI integration ( Maintain full compliance with the No Surprises Act ( Leverage price transparency and reference-based pricing tools Software that Rises to Any TPA’s Challenge Looking for a foundational partner to grow your business? Schedule a demo today. 908.813.3440 sales@hi-techhealth.com hi-techhealth.com
SELF INSURANCE INSTITUTE OF AMERICA, INC. 2023
BOARD OF DIRECTORS
CHAIRWOMAN OF THE BOARD*
Elizabeth Midtlien
Vice President, Emerging Markets
AmeriHealth Administrators, Inc.
Bloomington, MN
CHAIRMAN ELECT & TREASURER AND CORPORATE SECRETARY *
John Capasso
President & CEO
Captive Planning Associates, LLC
Marlton, NJ
DIRECTOR
Stacy Borans
Founder/Chief Medical Officer
Advanced Medical Strategies
Lynnfield, MA
DIRECTOR
Matt Kirk President
The Benecon Group
Lititz, PA
DIRECTOR
Mark Combs
CEO/President
Self-Insured Reporting
Greenville, SC
DIRECTOR
Shaun L. Peterson
VP, Stop Loss
Voya Financial
Minneapolis, MN
DIRECTOR
Amy Gasbarro
Chief Operating Officer
Vālenz
Phoenix, AZ
DIRECTOR
Adam Russo CEO
The Phia Group, LLC
Canton, MA DIRECTOR
Deborah Hodges President & CEO Health Plans, Inc.
Westborough, MA
COMMITTEE CHAIRS
Captive Insurance Committee
Jeffrey Fitzgerald
Vice President
Innovative Captive Strategies
Waukee, IA
Future Leaders Committee
Erin Duffy
Director of Business Development
Imagine360
Wayne, PA
Price Transparency Committee
Christine Cooper CEO aequum, LLC
Cleveland, OH
Captive Insurance Advocacy Task Force
Jeffrey K. Simpson
Partner
Womble Bond Dickinson (US) LLP
Wilmington, DE
Workers’ Compensation Committee
Shelly Brotzge
Regional Underwriter, Group Self Insurance
Midwest Employers Casualty
Chesterfield, MO
SIEF BOARD OF DIRECTORS
CHAIRMAN
Nigel Wallbank
Preisdent
Leadenhall, LLC
Ocala, FL
PRESIDENT
Daniél C. Kimlinger, Ph.D.
CEO
MINES and Associates
Littleton, CO
DIRECTORS
Freda Bacon
Administrator
AL Self-Insured Workers' Comp Fund
Birmingham, AL
Les Boughner
Chairman
Advantage Insurance Management (USA) LLC
Charleston, SC
Alex Giordano
Chief Executive Officer
Hudson Atlantic Benefits
Bellmore, NY
Virginia Johnson
Strategic Account Director
Verisk/ISO Claims Partners
Charlotte, NC
* Also serves as Director
OCTOBER 2023 81
SIIA NEW MEMBERS
REGULAR CORPORATE MEMBERS
Jesse Ohayon
CEO
Doctegrity
Plano, TX
Patrick Haig
CEO & Co-Founder
Goodbill
Dover, DE
Nandini Devi
Chief Executive Officer
Mpowered Health
Los Altos, CA
Chris Metcalf
VP Growth & Strategy
Prescription Care Management
Reno, NV
Betty Heiman
Founder And CEO
Transparent Health Group
Plainview, NY
Russell Pekala Cofounder
Yuzu Health
New York, NY
EVENTS
Healthcare Price Transparency Forum
February 26-27, 2024
Charlotte, NC
Artificial Intelligence Forum
February 27-28, 2024
Charlotte, NC
Spring Forum
March 25-27, 2024
San Antonio, TX
Future Leaders Forum
April 9-10, 2024
Kansas City, MO
Corporate Growth Forum
May 6-8, 2024
Greenville, SC
Cell + Gene Therapy Stakeholder Forum
May 29-30, 2024
Minneapolis, MN
SILVER MEMBERS
Michael Buesing
CEO
Buesing Consulting
Spring Hill, TN
John Walker
Business Development Specialist
ProAct, Inc.
East Syracuse, NY
Manny Odzakovic
Senior Vice PresidentUnderwriter and Actuary
Sompo International
Hamilton, Bermuda
International Conference
July 22-24, 2024*
Dublin, Ireland
National Conference & Expo
September 22-24, 2024
Phoenix, AZ
*tentative
OCTOBER 2023
82 THE SELF-INSURER

Connect with Zelis today at 888.311.3505 or visit zelis.com to get started. Save your clients money while improving their member experience? Doesn’t sound possible. But Zelis is delivering. We’ve saved over $27B in network and claim costs while helping healthcare carriers, TPAs, and self-insured employers modernize the healthcare financial experience. Zelis is your trusted partner to optimize financial performance and manage risk while delivering a great experience.
Catastrophic claims can arise unexpectedly. If the plan has the right Stop Loss protection in place, focus can remain on achieving business goals and welcoming Leo back when it’s time. When you work with the experts at HM Insurance Group, you can have confidence that the claims will be paid. Find more on hmig.com
Leo didn’t think he’d need heart surgery – or a second procedure two weeks later. Neither did his self-funded employer. MTG-3460 (11/22) *Cost estimate based on HM Insurance Group historical Stop Loss data and additional industry observations, October 2022. In all states except New York, coverage may be underwritten by HM Life Insurance Company, Pittsburgh, PA, or Highmark Casualty Insurance Company, Pittsburgh, PA. In New York, coverage is underwritten by HM Life Insurance Company of New York, New York, NY. The coverage or service requested may not be available in all states and is subject to individual state approval. SECURE FINANCIAL PROTECTION WITH OUR INSURANCE AND REINSURANCE OPTIONS: Employer Stop Loss: Traditional Protection • Small Group Solutions • Coverage Over Reference-Based Pricing Managed Care Reinsurance: Provider Excess Loss • Health Plan Reinsurance Life Is Not Without Risk.
An unexpected cardiac procedure with further corrective treatment could create claims of more than $800,000.*



 Matthew Drakeley Vice President, Specialty Markets
Matthew Drakeley Vice President, Specialty Markets

 By Bruce Shutan
By Bruce Shutan






 Marie Noble, MBA, AIC VP of Subrogation Management Marie.Noble@us.davies-group.com
Marie Noble, MBA, AIC VP of Subrogation Management Marie.Noble@us.davies-group.com




 Written By Bruce Shutan
Written By Bruce Shutan





















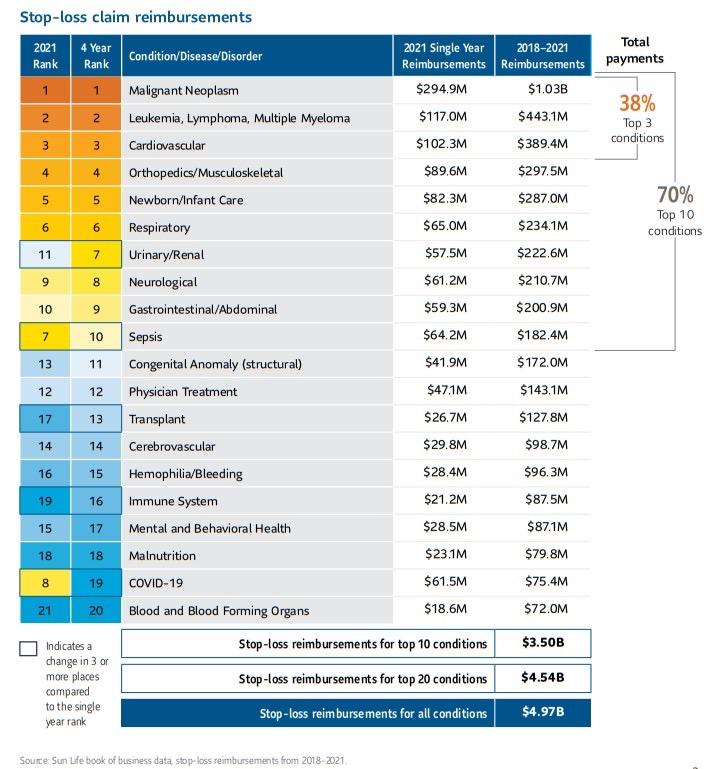








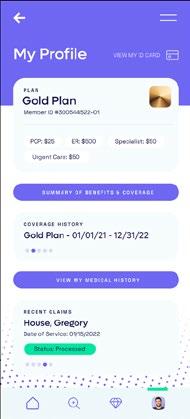
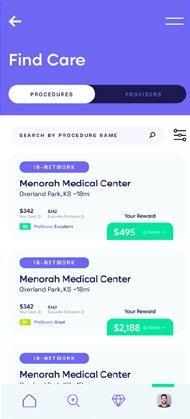
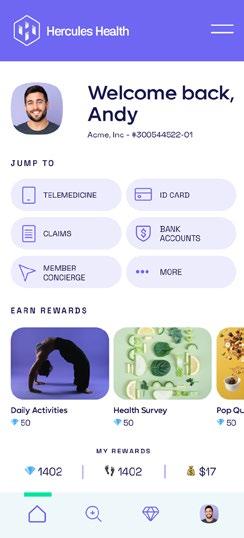









 Written By Kevin Brady, Esq., Director, Plan Document Compliance of The Phia Group
Written By Kevin Brady, Esq., Director, Plan Document Compliance of The Phia Group
















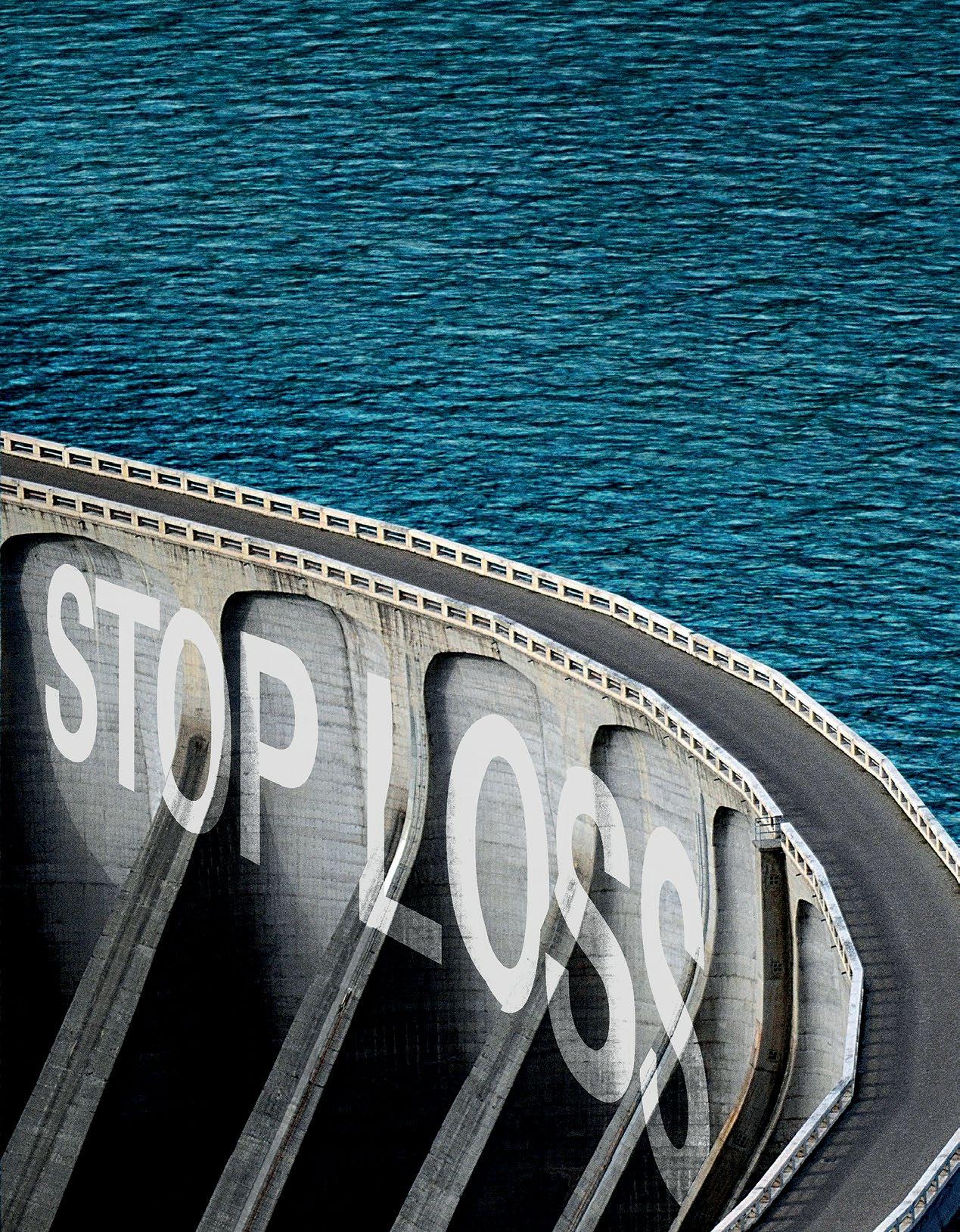






















 Proud to be a Diamond Member
Proud to be a Diamond Member