Price Transparency’s Hazy State
IN THE ABSENCE OF A STANDARDIZED DATA FORMAT, THE QUEST FOR USEABLE DATA IS STILL VERY MUCH A WORK IN PROGRESS


IN THE ABSENCE OF A STANDARDIZED DATA FORMAT, THE QUEST FOR USEABLE DATA IS STILL VERY MUCH A WORK IN PROGRESS

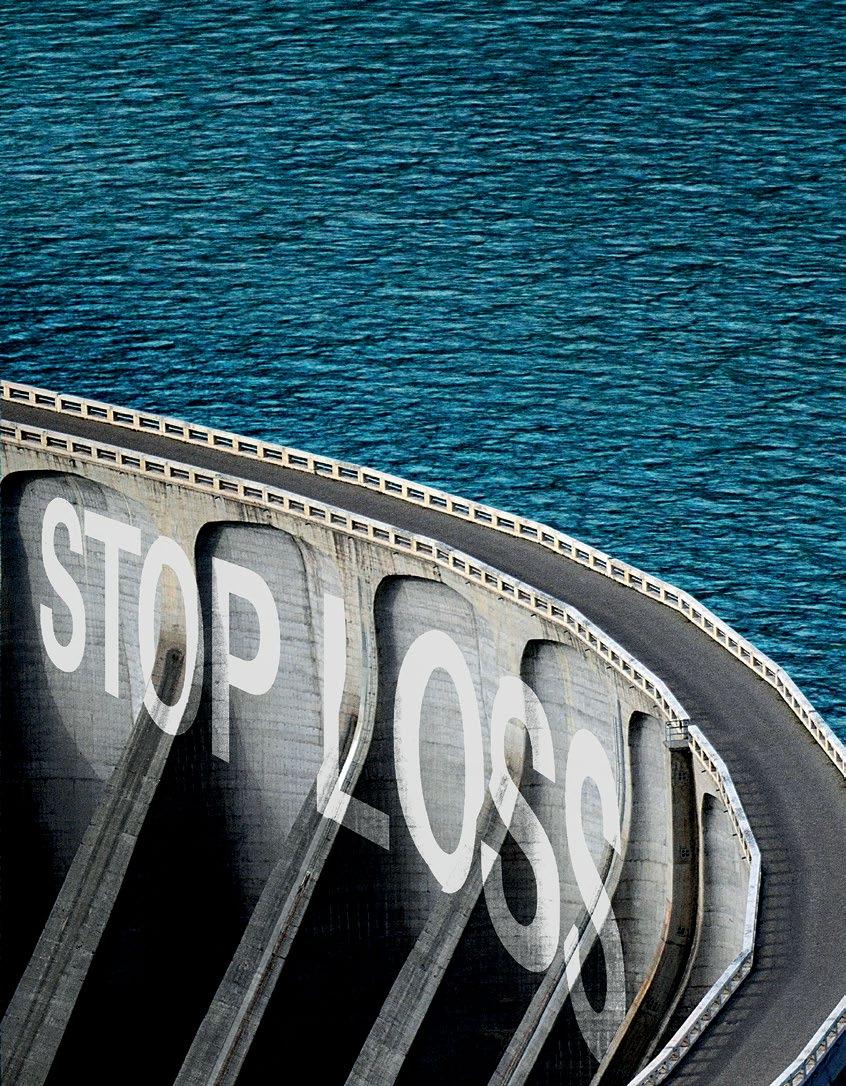
Self-insuring your healthcare benefits can be a big step for your company — and a complicated one. But with a medical stop loss solution from QBE, our experts will help you determine the level of risk protection to meet your financial needs.


Discover a range of products to help you protect your assets:
• Medical Stop Loss
• Captive Medical Stop Loss
• Special Risk Accident
• Organ Transplant
Together, we’ll create a solution so no matter what happens next, you can stay focused on your future.
Explore industry trends, insights and product details that can help you better manage the risks of a self-funded healthcare plan.
To learn more and read the full report, visit us at qbe.com/us/ah
4 PRICE TRANSPARENCY’S HAZY STATE IN THE ABSENCE OF A STANDARDIZED DATA FORMAT, THE QUEST FOR USEABLE DATA IS STILL VERY MUCH A WORK IN PROGRESS
 By Bruce Shutan
By Bruce Shutan
14 LONG COVID IS REAL: NEW CHRONIC CONDITION IMPACTS SELF-INSURED COMMUNITY CAN SELF-INSURED HEALTH PLANS HELP MEMBERS UNDERSTAND THE FLOW?
 By Laura Carabello
By Laura Carabello
The Self-Insurer (ISSN 10913815) is published monthly by Self-Insurers’ Publishing Corp. (SIPC). Postmaster: Send address changes to The Self-Insurer Editorial and Advertising Office, P.O. Box 1237, Simpsonville, SC 29681,(888) 394-5688
PUBLISHING DIRECTOR Erica Massey, SENIOR EDITOR Gretchen Grote, CONTRIBUTING EDITORS Mike Ferguson and Ryan Work, DIRECTOR OF ADVERTISING Shane Byars, EDITORIAL ADVISOR Bruce Shutan, 2023 Self-Insurers’ Publishing Corp. Officers James A. Kinder, CEO/Chairman, Erica M. Massey, President, Lynne Bolduc, Esq. Secretary

Datadrives decision-making in health care, but it’s not always readily available – even in the face of mandates.
More than a year after the No Surprises Act became law and seven months since the Transparency in Coverage (TIC) final rule took effect, industry observers say that while health care pricing is becoming more transparent, a seemingly bright landscape is still clouded by perverse practices. Two chief culprits have emerged: the absence of a standard format that enables apples-to-apples data comparisons and lack of federal enforcement, which has fueled noncompliance.
Whereas anywhere from 40% to 65% of hospitals are said to be fully compliant with the TIC, higher fines for violations will serve as an incentive for them to offer transparent pricing data that’s understandable and useful to consumers, opines Dawn Cornelis, cofounder of Claim Informatics.

A Deloitte survey showed that 60% of consumers are more than likely to choose a provider that publishes local rates on their services, she noted. Yet a Harvard study indicated 75% of consumers do not know that there’s even health care pricing tool available.
Therefore, Cornelis says the focus needs to be on promoting better awareness of health care price transparency and empowering consumers to use these tools to make more cost-effective choices that eventually will help drive down inflated prices across the market.
years of hospital and physicians’ claims processed within the Medicare program. They’re trying to overcomplicate things with barriers and hospital systems are known for that. We need to dumb it down and say, ‘it’s not that complicated to put together a standard record format layout that everybody follows.’”
With access to transparent pricing on hospital websites in shoppable form and the ability to actually see price variations, facilities will find it much harder to justify higher prices for the exact same procedure, services, supplies and even doctor, Cornelis says.
Despite the TIC, many hospitals continue to make a lot of information available in “a very unusable format” that the average patient struggles to understand when deciphering various medical procedures, benefit levels and out-of-pocket costs, observes Dave Cardelle, chief strategy officer of AMS.
While he believes some have done it intentionally, others have made it “super complicated for that data to be easily usable because CMS didn’t provide any standard format.” The result is a free for all involving confusing information floating around the marketplace with hospitals publishing machine readable files that meet certain requirements, but make meaningful comparisons an uphill battle.
Having worked with data for 35-plus years, Cornelis knew the TIC was flawed from the start. “It becomes complicated when people want to make it complicated,” she quips. “I heard the single month of UnitedHealthcare’s pricing transparency data is larger than three full

But until systemic issues can be resolved, the future of price transparency will continue to hang in the balance. While the intent of this new regulatory environment was to make the marketplace more competitive, Cardelle cautions that hospitals still monopolize certain regions of the country. “I don’t know that it’s going to really move the needle as far as changing prices for a lot of the hospitals that are out there,” he says.
Still, the TIC is a good start that will require patience. As with any undertaking of this enormity, much can change between version 1.0 and 5.0 in the emerging health care price transparency
“It really is going to come down to employers that want to use price transparency in coverage to their advantage,” she says.
“They need to put together a team to help employees navigate the rules, as well as the CAA [Consolidated Appropriations Act] guidelines.”

When it comes to keeping compliant with the No Surprises Act, don’t play it by ear. Administrators need a flexible solution for Transparency, and IPS is here to fine-tune your compliance plan.
Transparency+ is the most efficient and inexpensive solution to meet all current and future regulations of the No Surprises Act. It fulfills all key components required by the NSA for Machine-Readable Files, Price Comparison Tools, Advanced EOBs, and Qualifying Payment Amounts.
Unparalleled
Bolt-on solution that can integrate with any existing tech stack
60-day average implementation to meet requirements fast
marketplace, according to Bill Kampine, chief innovation officer of Healthcare Bluebook.

quality metrics empowers patients to make decisions that balance cost and quality in both inpatient and outpatient settings.
he says, noting that the intent was not be overly prescriptive beyond having certain elements in place to protect consumers. Rather, the thinking was that market innovators would eventually determine the clearest way of presenting shoppable information.
That starts with an ability to contextualize the volumes of data in ways that Kampine says are meaningful to patients. For example, surgeries will have multiple components that include the surgeon, anesthesia, facility and potentially other charges. In order to avoid surprise bills, he says patients need accurate and thorough estimates for the complete encounter, as well as benchmarks on key decisions that will have the greatest impact on cost such as the choice of facility.
What’s critical for obtaining value is presenting consumers with a complete list of providers, prices and available alternatives, Kampine notes. One example is that the hospital transparency rules apply to a limited list of procedures, many of which include outpatient care that can be delivered in far less costly settings such as a provider’s office, ambulatory surgery center and independent imaging center.
Having that data doesn’t guarantee lower cost and better outcomes, he cautions, adding that benefit design is still “the most powerful tool plan sponsors have at their disposal for achieving improved value.” A proven model for lowering his client’s health care costs features intuitive, easily accessible price and quality information from high-value providers, as well as concierge level navigation support.
In terms of improving the data that’s currently available, Cardelle believes it wouldn’t take long to build consensus. “All basic
contain
same primary information so the government can set out a simple data
Price, of course, is only one data point. “Quality is equally important and not part of the federal price transparency requirements,” Kampine points out. He says risk adjusted, patient-specific outcomes based

“The progress that occurs between these versions incorporates feedback and learnings to make it more functional over time,”
“Looking up prices one hospital at a time is time consuming, and could still lead to overpayment if the consumer cannot directly compare prices for the same service across all available settings,” he adds.
chargemasters
theDave Cardelle
One huge benefit from the TIC is that the curtain has finally been pulled back on cash pricing, which providers have quietly accepted. Health plans can now start to see what the hospital’s chargemasters are in discounted cash prices and use that information as a comparison to what they’re paying, he explains.
What’s most important, in his view, is that hospitals are actually willing to accept cash prices, which should be a baseline for every single service on their chargemaster, “and then from there, hospitals should be able to negotiate discounts off of that price.” This is especially critical for patients who have no health insurance.
on some of the discrepancies and variances, he adds.
Since hospital data is so massive, the information must be curated by experts for any useful comparisons, according to Cardelle. Examples include the involvement of a thirdparty software or data analytics vendor to download files, uncover discrepancies and aggregate the information for practical use. His firm already has downloaded more than 6,000 files from 5,600 hospitals. With over 5 million
The TIC is now shining a light
We’re passionate about providing a stress-free experience through a collaborative, listening approach.
Marketing Stop Loss
Our specialized teams can provide guidance and service in areas like:
• Plan performance analysis and consultation
• Regulatory requirements and compliance
• Stop Loss options
Compliance Concierge
• Marketing and communications
• Full-service concierge and navigation tools
• Clinical management
• Custom-built, scalable plans
Reporting Clinical Management
Not just a TPA, a partner.
hpiTPA.com
But the marketplace isn’t there yet. “We have seen examples where health plans actually pay five times with the cash prices, which makes no sense whatsoever,” he reports.
From locally-focused to national-scale programs, AmeriHealth Administrators offers a full spectrum of third-party administration and business process outsourcing services. Our scalable capabilities service many unique customers, including self-funded employers, Tribal nations, international travelers, and labor organizations.
We offer innovative solutions, insight, and expertise to help you manage your health plan and capabilities, control costs, and support employees’ health.
Visit amerihealth.com/tpa

unique codes and approximately 5 billion line items to pore through, he says the data “becomes just unruly, but that information is super valuable.”
Adds Cornelis: “There is a cottage industry for taking large sets of data, but it has to be with empathy – that there’s no conflict of interest or some other objective going on.” Her firm has built a technology platform that allows patients to decipher the average cost of various procedures from large sets of complicated healthcare claims data.
If there’s anyone who can truly relate to the level of mounting frustration among health care consumers over opaque pricing, it’s Cornelis. When she recently underwent a kidney stone removal, it dramatized just how difficult it is for even a subject matter expert to navigate her way through a complex health care system.
We would like to invite you to share your insight and submit an article to The Self-Insurer! SIIA’s official magazine is distributed in a digital and print format to reach 10,000 readers all over the world.
The Self-Insurer has been delivering information to top-level executives in the self-insurance industry since 1984.
Articles or guideline inquires can be submitted to Editor Gretchen Grote at ggrote@ sipconline.net
But as Cornelis and others agree, there’s reason to believe that the forecast for health care price transparency will likely become brighter over time.
Bruce Shutan is a Portland, Oregon-based freelance writer who has closely covered the employee benefits industry for more than 30 years.
The Self-Insurer also has advertising opportunties available. Please contact Shane Byars at sbyars@ sipconline.net for advertising information.

“I called probably five different numbers and nobody could answer my question about getting a price for this procedure,” she reports.
“I knew the facility and who the surgeon was, and I struck out at the hospital, carrier and network. I couldn’t get anywhere. That’s the reality that sets in when we start looking at the price transparency rules.”

Federal regulators are forcing the health care marketplace to offer transparent pricing, but self-insured health plans will continue to encounter some landmines along this changing landscape.
Mindful of the need to reduce balance billing and litigation under the No Surprises Act (NSA), a recently issued final rule is helping implement the independent dispute resolution (IDR) process. It features “baseball-style” arbitration between payers and providers through which both sides offer a payment amount.

The IDR entity picks one of those amounts rather than split the difference, although the two parties involved still can continue to negotiate or strike a settlement. The trouble is IDR entities are “massively understaffed and not really following the rules because there’s just not enough time for them to do so based on the volume of claims,” cautions Christine Cooper, CEO of aqueem LLC.
At the center of NSA arbitration is a qualifying payment amount (QPA) that serves as the basis for determining cost sharing for items and services covered by the 13-month-old law’s balance-billing protections.
Prior to the release of any IDR guidance, Cooper says providers were grumbling how it’s unfair that the QPA is calculated by the TPA, health plan and insurers “because it’s their information that we don’t even have access to, so there is no transparency and to them it’s a very arbitrary number.”
While the Centers for Medicare & Medicaid Services estimates that arbiters deemed at least 22,000 disputes ineligible for IDR, all eyes are on the U.S. District Court for the Eastern District of Texas where arguments were heard in the second of three lawsuits by

“When you’re an IDR entity with however many thousands of these claims streaming in, how do you have the time to sit back and look at all seven factors, then prepare a written decision and actually get through these IDR claims?”
the Texas Medical Association (TMA) challenging portions of the rule. TMA sought to eliminate the interim final rule provision that allows a self-insured plan to use data across their TPA for QPA calculations.
The location of this legal battle proved to be a calculated and strategic move on behalf of the provider community, according to Cooper, who points out that providers were wise to sue in the Lone Star State where the climate has been favorable for them.
Another significant factor to consider is whether the health plan employs reference-based pricing. “From an RBP standpoint,
high,” says Troy Sisum, chief legal officer at Imagine360. His company has been able to negotiate and resolve eligible claims below the QPA by accessing enough data and supportable documentation to suggest what the plan paid is reasonable. He notes that it’s important to have arbiters use the QPA as a good starting point because it’s something that can be audited.

The NSA litigation impacts BUCAH plans a little more than RBP, Sisum believes, “because it potentially can allow providers to file more IDR challenges, where I think a lot of the BUCAHs were betting that if they just pay the QPA, they really wouldn’t see many of these IDRs. And I think that that didn’t materialize the way they had hoped.”
Just as with the Affordable Care Act, Cooper sees a long road ahead for unfolding legal battles under the NSA. “We’re only seeing the beginning of this litigation,” she observes, advising employers to take steps in the plan design to avoid the NSA in the first place. “I think the Administrative Procedures Act is going to play a central focus in the litigation in the sense of HHS, Department of Labor and others involved in this rulemaking really overstep their bounds.”
Bruce Shutan is a Portland, Oregon-based freelance writer who has closely covered the employee benefits industry for more than 30 years.
you want to be able to negotiate and go to IDR and argue that the QPA is too
Justwhen everyone was starting to relax about the impact of COVID-19 on the workplace, it appears that it’s a long way from over.
Long COVID is a chronic illness that results from a Covid-19 infection and there are hundreds of potential residual symptoms or medical complications which can be debilitating for many people.
The Centers for Disease Control and Prevention (CDC) reports that millions of people suffer from Long COVID and David Cutler, an economist at Harvard University who projected the $3.7 trillion economic cost of Long-COVID estimates the individual medical costs of the disease to be about $9K+ a year, on average.

This does not include key treatment regimens for hospitalization as well as the indirect costs of workforce absence and potential patient disability.
Paul Fallisi, FSA, MAA, president, Windsor Strategy Partners, a leading actuarial firm, advises, "LongCovid is basically a new chronic condition requiring ongoing medical attention like high blood pressure, diabetes and obesity. It will affect claims morbidity for the foreseeable future! Fingers crossed that future variants of Covid-19 are mild – but extreme variants are a complete morbidity wild card.”
He points out that from 2020 through 2021, COVID-19 claims were offset by fewer doctor visits. Emergency Room visits, elective surgeries and dancer screenings, noting, “But going forward, 2023 total claims will be impacted by COVID-19 and Long COVID claims not offset by fewer physician office visits. Additionally, medical inflation will be higher due to higher general inflation and the addition of Long COVID claims and cancer claims will be higher due to delayed screenings and treatments. Unfortunately, cancer claims will be more expensive due to later than normal detection.”
Most Common Symptoms of Long COVID
• Coughing
• Ongoing, sometimes debilitating, fatigue
• Body aches
• Joint pain
• Shortness of breath
• Loss of taste and smell — even if this did not occur during the height of their illness
• Difficulty sleeping
• Headaches
• Brain fog: patients report being unusually forgetful, confused or unable to concentrate even enough to watch TV.
Source: UC Davis Health
Long COVID poses a significant business concern with broader workforce implications. It continues to alter the employment landscape, with the American Medical Association (AMA) estimating that 10-30% of the 81 million people diagnosed with COVID will develop long COVID, for months or years to come.
Fallisi reports that 13.3% of people that have had COVID-19 experience some of these symptoms one month after infection, 2.5% of these people experience some of these symptoms three months after infection and 30% of the people that were hospitalized for COVID-19 experienced some form of Long COVID six months after infection.




It should be noted that Post-COVID conditions are found more often in people who had severe COVID-19 illness, but anyone who has been infected with the virus that causes COVID-19 can experience post-COVID conditions, even people who had mild illness or no symptoms from COVID-19.
While most people with post-COVID conditions have evidence of infection or COVID-19 illness, in some cases, a person with postCOVID conditions may not have tested positive for the virus or known they were infected.
Given these statistics, astute employers need to understand their social and legal obligations to their employees. Failure to do so can be costly to employers directly from discrimination lawsuits, workplace injuries or other liability for other accidents caused by employees or product liability from substandard production.
There’s also the indirect costs to re-hire or retrain workers. Long COVID can result in continued disruptions and financial implications long into the future.
Jakki Lynch RN, CCM, CMAS CCFA, director cost containment, Sequoia Reinsurance Services says,
She explains that some patients, especially those who had severe COVID-19, have persistent heart, kidney, liver, and nervous system issues and even permanent damage to multiple organs requiring ongoing costly health treatment interventions.

Lynch cites these important studies:
A study published in 2020 in the journal JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation.
According to C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine in Baltimore, nearly a third of patients hospitalized for COVID-19 experienced kidney damage that may become chronic; some may need dialysis or a transplant.
According to United Network for Organ Sharing, the private, nonprofit organization that manages the U.S. organ transplantation system, total US
“Plan sponsors have become acutely aware of the financial impact that Long-COVID has on their plan spend. LongCOVID is challenging and costly for several reasons; an official Long-COVID diagnosis can be difficult as there is no specific test to diagnose post-COVID conditions and treatment largely consists of symptom management rather than evidence-based treatment protocols which can be labor intensive and long-lasting ranging from three months to a year or more.”
transplant volume is trending upward among the working age group during the pandemic (despite a temporary dip in transplants early in 2020) compared to pre-pandemic volume.
Total costs for organ transplant are also increasing for solid organ transplants year-over-year with claims for a single transplant often exceeding $1 million, in particular lung and heart transplants per Milliman’s 2020 triennial report.
“Plan sponsors need affordability solutions to manage Long-COVID high risk expenses and maintain access to timely care,” she continues. “The key interventions to help manage this novel financial exposure include:
1) Promotion of best practices for prevention and early intervention strategies for treatment of COVID-19through proactive patient and provider communication.
2) Access to resources and proactive referrals to multidisciplinary specialist physician teams that focus on the treatment of Long-COVID.
3) Provider contract reimbursement analysis and targeted updates to address the unique risks and nuances of LongCOVID treatments.
4) Claim payment integrity reviews which ensure correct reimbursement and accurate payment of plan benefits.”

Medical Stop Loss from Berkshire Hathaway Specialty Insurance comes with a professional claims team committed to doing the right thing for our customers – and doing it fast. Our customers know they will be reimbursed rapidly and accurately – with the certainty you would expect from our formidable balance sheet and trusted brand. That’s a policy you can rely on.
right. www.bhspecialty.com/msl
Here's some good advice from Jack Towarnicky, member, aequum LLC, an ERISA/Employee Benefits compliance and planning attorney, “Long COVID occurs when symptoms last over 30 days. The CDC estimates that 23 million Americans suffered long COVID, incurring hundreds of billions of medical expenses, and as stated above, the $9,000 per patient estimated expense doesn’t include lost wages or short and long-term disability benefit costs.”
Towarnicky points out that employee-patients also suffer financially:
• Where treatment stretches into 2023, most will have to satisfy another annual deductible,
• Sick leave, short and long-term disability benefits often don’t replace 100% of pre-disability wages, and
• Should long COVID continue for 12 weeks, some will lose employment and employer-sponsored coverage.

Employers should also be aware that as of July 2021, long COVID can be considered a disability under the Americans with Disabilities Act. To avoid lawsuits, it is advisable to educate and train managers since there may be no visible or outward signs of disability.
When an employee requests an accommodation related to this disability, management should determine if a reasonable accommodation could or should be made.
The long-term impact of the virus is complicating injured worker recoveries, impacting insurers and insureds’ ability to project claim costs. A growing number of patients -- “Long COVID” or “long haulers” --- will experience mild to moderate symptoms for a prolonged period of time.
With the relatively high concentration of COVID-19 workers compensation claims in the healthcare industry, this is regarded as an important development that merits monitoring. Amid this uncertainty, employers may be advised to know and prepare for these eventualities, as the uncertainty of long-term COVID-19 continues to be studied and evaluated.
Workers’ Comp experts at Liberty Mutual project:
1. COVID-19 claims are likely to be unique, not straightforward
With all the uncertainties of COVID-19, a common denominator seems to be that it can affect everyone differently. While some people return to normal fairly quickly, others experience a volatile recovery that includes relapses, and can take several weeks. Each COVID-19 occurrence may have distinct consequences – continuing to challenge riskplanning and complicating claimcost calculations over the long term. One study finds that the chance of full recovery from COVID-19 infection by day 50 is less than 20% for patients with prolonged symptoms.
2. COVID-19 claims may have long tails, with full impact unknown until later
Because some healthcare employers have scaled back operations at various points of the pandemic with workers logging fewer hours, working remotely, or being furloughed, they may see a modest decrease in the number of annual workers compensation claims, and, as noted above, the majority of COVID-19 claims have not been severe.
But concerns remain about the potential challenge that both employers and insurers may face with the long-tail nature of COVID-19 claims. According
to the “2020 State of the Line Guide” by the National Council on Compensation Insurance (NCCI), there are several aspects that could easily extend active claims, including:
• Severity of illness will dictate costs – from lowcost medical care to treat mild symptoms, to hospital stays and/or extended rehabilitation for more serious cases;
• Delayed medical care and physical therapy for other non-acute conditions may contribute to injury creep – extending claim duration and putting upward pressure on costs; and
• Some COVID-19 claims may also involve a mental component and could require temporary or long-term treatment.
As a result, say the experts, premiums collected today must cover losses for years to come and significantly impact the cost of insurance.
3. COVID-19 experiences pose challenges to return-to-work norms and staffing
A key part of managing workers compensation costs is ensuring timely medical care in order to support return to work as quickly and safely as possible after recovery. But with delays and reductions in elective procedures, as well as patients delaying care and reducing their healthcare spending, the industry has seen broad furloughs and layoffs; workers on leave may not have jobs to which they can return. Fewer return-to-work and light-duty opportunities may be available, which could also boost claim duration.
In a recent survey by Milliman, more than 40% of hospital, clinic, home care, and long-term care organizations are encouraging employees who test positive for COVID-19 to apply for workers compensation if there is known occupational exposure. About 32% are providing other leave benefits such as quarantine pay and short-term housing.

Industry consultants also advise that Long COVID may create safety issues. Employers recognize a general duty to provide a safe working environment for their employees, as mandated by OSHA. But with potentially 24 million employees suffering from Long COVID symptoms, there may be an increased risk of workplace injuries and accidents.
This may be especially relevant in heavy labor industries or any industry with driving exposure where chronic fatigue, brain fog, and other long COVID symptoms present an intrinsically greater risk of employees sustaining an injury to themselves, co-workers or even the public.
Since there is no test to diagnose post-COVID conditions, and there is a wide variety of symptoms that could come from other health problems, it is difficult for healthcare providers to recognize postCOVID conditions.
Nevertheless, the AMA adopted a policy supporting “the development of an ICD-10 code or family of codes to recognize Long COVID (also known as post-acute sequelae SARS-CoV-2 infection or PASC) and other novel post-viral syndromes as a distinct diagnosis.”
Symptoms of Long Covid may go unrecognized as employees unknowingly suffer and find that they are experiencing issues such as chronic fatigue, brain fog, mental illness, chronic shortness of breath, migraines and other complex medical conditions that impact their ability to work.
It appears that Long COVID conditions align with the severity of infection. A new study in the Journal of Internal Medicine based on records for roughly 200,000 patients in Sweden describes who is diagnosed with a new condition and who had one before. Diagnoses tracked with illness severity, but there were other factors: females and those diagnosed with previous mental health disorders or asthma were more likely to have post Covid-19 conditions among nonhospitalized and hospitalized individuals.
Before acute infection, 53% of non-hospitalized, 48% of hospitalized, and 41% of ICU-treated individuals had one or more diagnoses that fit under the post-Covid condition umbrella, most often anxiety for nonhospitalized (16%) and hospitalized (12%) people and muscle pain (12%) for the ICU patients. The authors suggest “some of the disease burden could be wrongly attributed to Covid-19 or that Covid-19 accentuates pre-existing conditions.”
Avivit Ben-Aharon, founder and clinical director, Great Speech, a leading virtual speech therapy company, explains, “Brain fog and memory issues are among the wide range of concerns that plague individuals in their recovery of long COVID. These issues include cognitive impairment, and/or speech and language difficulties. Speech therapy provides an effective means to address such conditions-- helping patients who are affected by long COVID to confidently return to work, handle daily life and resume an active lifestyle.”
She says that virtual speech therapy provides the added benefits of allowing people to get help from the comfort of their homes or at work during their lunch break, “These benefits eliminate travel to an off-site brick-and-mortar facility and minimize opportunities for exposure of viruses and illnesses.”




One quip that is circulating in the industry: “If you never get COVID-19, you will never suffer with Long COVID.”
To this point, NPR reports that the Centers for Disease Control and Prevention (CDC) warn two new omicron subvariants have become dominant in the United States, raising fears they could fuel yet another surge of COVID-19 infections. The subvariants — called BQ.1 and BQ.1.1 -- appear to be among the most proficient at evading immunity from vaccination and previous infection.
As a result, winter 2023 may cause workforces to experience higher rates of absenteeism and health problems as more employees call in sick to care for themselves and families. Many experts advise that routine COVID testing remains a vital way to limit the number of cases that hit workforces since even a mild SARS-CoV-2 infection can cause long COVID.
Analysts caution that people who are not vaccinated against COVID-19 and become infected might also be at higher risk of developing post-COVID conditions compared to people who were vaccinated and had breakthrough infections.
Source: STAT. December 14, 2022
A new CDC report is disheartening: long COVID and other names for symptoms that persist after acute infection are appearing on death certificates in a small percentage of people who have died during the pandemic.
Harlan Krumholz, a Yale cardiologist who has been working with long COVID patients, says, "…the challenge is that the data they have provides only a floor of an estimate of the mortality burden of long Covid," including suicide.
Other experts say the CDC numbers are at best an undercount and at worst represent a “myopic” view of people living with Long COVID. The report also notes disparities in Long COVID deaths that reflect the pandemic overall. In addition to the death rate being highest among adults 85 and older and among men compared to women, non-Hispanic American Indian or Alaska Native people had a death rate that was more than twice as high as people from other racial or ethnic groups.

David Putrino, director of rehabilitation innovation at Mount Sinai Health System, expresses a troubling perspective that only emphasizes severe acute infection.
says Putrino, who started one of the first Long
“We're still being incredibly myopic about our viewpoint of what long Covid is. And so we're not studying all of the ways that it is causing loss of life,”
COVID clinics in the U.S.
This backdrop of “gloom and doom” has actually contributed to the creation of some very positive initiatives. The Long COVID Research Consortium was established as a scientific collaboration to rapidly and comprehensively study the condition, including scientists and clinicians from venerable institutions. including Harvard Medical School, University of California San Francisco, the J. Craig Venter Institute, Johns Hopkins, University of Pennsylvania, the Icahn School of Medicine at Mount Sinai, Cardiff University and Yale University.
They say it is no longer a mystery, with new research revealing key drivers of the condition, including evidence strongly suggesting that patients with Long COVID do not fully clear the SARS-CoV-2 virus. Instead, the virus may persist in tissue where it continues to provoke the immune system, driving a wide range of downstream consequences such as blood clotting, neuroinflammation and neuropathy.
One study from the Medical University of Innsbruck set out to look for molecular traces of virus in the gut, which is considered a favorite ‘hunting ground’ for researchers studying SARS-CoV-2. Of the 46

“It's very, very clear that the majority of these cases were related to individuals who had severe acute disease and were struggling to recover from severe acute disease. The truth is, there are many, many more — orders of magnitude more — folks who initially did not have severe acute disease but went on to develop these highly debilitating symptoms.”
people who’d had COVID-19 months earlier, 21 of whom had at least one symptom of Long COVID.
The bottom line of the study published in May in Gastroenterology: all of those with Long COVID symptoms harbored viral RNA or, in some cases, viral proteins. Among those who’d recovered from acute COVID-19, 11 had traces of virus, too, whereas another 14 had no virus that researchers could find.
In the United States, microbiologist Amy Proal, a microbiologist with expertise in pathogen persistence who serves as president and chief scientific officer of the PolyBio Research Foundation. says she can’t stop thinking about a second leading Long Covid theory: that the coronavirus keeps hurting people by stubbornly enduring in the body, even after acute infection passes. She reports that studies have shown “the virus is capable of persistence in a wide range of body sites,” especially nerves and other tissues. Proal has had COVID-19 three times and asserts, “I consider Long COVID to be a massive emergency.”
Laura Carabello holds a degree in Journalism from the Newhouse School of Communications at Syracuse University, is a recognized expert in medical travel, and is a widely published writer on healthcare issues. She is a Principal at CPR Strategic Marketing Communications. www.cpronline.com
References:
https://polybio.org/longcovid
https://www.science.org/content/article/what-causes-long-covid-three-leadingtheories#:~:text=The%20bottom%20line%3A%20All%20of,study%20in%20May%20in%20 Gastroenterology.https://www.cnbc.com/2022/12/01/long-covid-costs-patients-an-average9000-a-year-in-medical-expenses.htmlhttps://fortune.com/2022/12/05/long-covid-millionsworkforce-170-billion-wages-employees-flu-season/
https://www.benefitspro.com/2022/05/23/what-employers-should-know-about-long-covid/
https://search.yahoo.com/search?p=long+covid+hurting+employers&fr=iphone&.tsrc=apple
https://www.benefitnews.com/news/why-employers-need-to-reinstate-covid-testing-policies
https://business.libertymutual.com/insights/3-impacts-of-long-term-covid-19-on-workerscomp-claims-healthcare-employers-need-to-know/
https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
https://www.npr.org/sections/health-shots/2022/11/11/1136039817/new-omicron-subvariantsnow-dominant-in-the-u-s-raising-fears-of-a-winter-surge
https://onlinelibrary.wiley.com/doi/10.1111/joim.13584?utm_source=STAT+Newsletters&utm_ campaign=b4c972cf41-MR_COPY_01&utm_medium=email&utm_term=0_8cab1d7961b4c972cf41-151821581
https://www.ama-assn.org/delivering-care/public-health/what-long-covid
https://health.ucdavis.edu/news/headlines/covid-19-long-hauler-patients-search-for-answersand-help/2020/10
https://www.statnews.com/2022/12/14/long-covid-death-certificate-records/?utm_ source=STAT+Newsletters&utm_campaign=3524aa216a-MR_COPY_01&utm_ medium=email&utm_term=0_8cab1d7961-3524aa216a-151821581
https://www.bloomberg.com/news/articles/2022-12-14/long-covid-immune-effects-seenlinked-with-high-global-deaths

 Written By Ryan Work, Senior Vice President, Government Relations Self-Insurance Institute of America, Inc. (SIIA)
Written By Ryan Work, Senior Vice President, Government Relations Self-Insurance Institute of America, Inc. (SIIA)
Shortlyafter the U.S. Supreme Court issued its decision in Marietta v. DaVita this past summer, dialysis providers and their allies were quick to introduce legislation that would have had a number of negative impacts and consequences for self-insured health plans. At the time, I didn’t realize just how much the SIIA government relations team would learn about dialysis policy, and politics, over the course of the next few months. This is the story of that advocacy campaign, and the dark side of what a dysfunctional provider system means for patients, plans and members.
First, a bit of context. Under a competitive healthcare space, innetwork provides choice and lower cost. It’s ‘usually’ good for plans, for patients, and it creates a known and agreed upon price. I say usually because in the case of dialysis it’s simply not the case.
While Medicare reimburses dialysis at $264 per treatment, self-insured plans pay an average reimbursement rate of $1,500. Rather than plans or patients having a number of providers to choose from and negotiate with, the dialysis space is a duopolytwo providers have approximately 80% of the market.
When that happens, that duopoly dictates and drives up prices, and creates a non-functioning network. As an example, while 12% of dialysis are on group health insurance, they account for 40% of provider revenue.
This positioning was the first major problem. In actuality, the Supreme Court decision didn’t change the status quo, rather it kept in place the three-part patient protections already enshrined in the Medicare Secondary Payer Act (MSPA), while allowing self-insured plans the ability to create lower cost reimbursement mechanisms through out-ofnetwork programs or improved in-network rates.
Dialysis, along with ALS, are the only conditions that qualifies an individual for Medicare coverage regardless of age. The specifics of this coverage is spelled out in the MSPA, which mandates that employers are the primary payor for what amounts to the first 33-months of care.
During this initial coverage period, employers are prohibited from dropping coverage for those dialysis patients under their plan, something that employers and regulators take seriously. After 33-months, Medicare then becomes the primary payer.
In August of this past year, SIIA became aware of legislative text being circulated by a large dialysis provider that sought to enshrine special protections for their ability to further control the dialysis market.
This legislation framed these special protections as parity standards for employer plans which would tie dialysis coverage benefits to coverage benefits for other chronic disease. This proposed legislation followed a Supreme Court decision on the issue of plans’ ability to control dialysis costs. Providers didn’t like the revenue impacts of this decision and were looking for a solution from Congress, claiming the decision created a new market dynamic.

The second major problem was the actual text of the legislation. If we learned anything over the past several years, it’s that mandating parity in health care is complex and difficult, and simply doesn’t work as intended. Different patients need different care, and ERISA provides flexibility to make that happen.
The mislabeled search for parity attempted to equate dialysis benefit coverage to that of other ‘chronic’ diseases.” While that is noble thought in the abstract, in the concrete, there is no way to make that work, starting with the fact that there is no federal definition of chronic diseases. One can only imagine the chaos caused by mandating coverage for something that isn’t defined.
Having identified those three major issues with the proposed legislation – misdirection, lack of practicality, and an undermining of basic flexibility – it was no surprise that just a week after introduction week later, Politico came out with an investigative piece citing the fact that DaVita itself wrote the legislation and had it introduced by allies on the Hill with no input or changes prior to introduction.
Third, the legislation would have forced self-insured plans to only use in-network rates as the only way to attempt to control dialysis costs. Such a restriction would eat away at the very foundations of ERISA, curtailing the very flexibility that is at the heart of self-funded health plans and preventing the use of cost containment resources, whether reference-based pricing or carve-out methodologies.
Dialysis providers are very active on the political and legislative fronts. Through September of 2022, DaVita spent over $3 million in lobbying, with Fresenius spending $5.65 million, in addition to millions in political contributions.

Dialysis providers were quick to use the patient groups they underwrite to start grassroots campaigns to boost support in Congress on their legislation, which was introduced as the Restore Protections for Dialysis Patients Act.
According to dialysis advocates misdirection, employers were using the Supreme Court decision to “kick patients off plans,” make sure they didn’t have to pay for their dependents and “dump” dialysis costs on to Medicare.
In addition, they claimed that the Justice Kavanaugh’s opinion in the Marietta case gutted the patient protections under the MSPA. The

Behind every claim is a person facing a health challenge. By supporting members in the moments that matter, we can improve health outcomes and help employers manage costs.
For nearly 40 years, self-funded employers have trusted Sun Life to quickly reimburse their stop-loss claims and be their second set of eyes, looking for savings opportunities. But we are ready to do more to help members in the moments that matter. We now offer care navigation and health advocacy services to help your employees and their families get the right care at the right time – and achieve better health outcomes. Let us support you with innovative health and risk solutions that benefit you and your medical plan members. It is time to rethink what you expect from your stop-loss partner.
Ask your Sun Life Stop-Loss Specialist about what is new at Sun Life or click here to learn more!
problem? None of this dangerous rhetoric was true. There is no data to demonstrate that plans are removing dialysis patients, and it’s illegal under three distinct federal laws.
Additionally, the healthcare space doesn’t move that fast, nor can plans change benefits or documents mid-year. In fact, not only is there no data to prove this accusation, but any data showing changes in the dialysis market may take years to come to light.

and trade coalitions, and with SIIA member companies.
According to the government’s own data in the U.S. Renal Dialysis Database, dialysis patients receiving coverage under Medicare has decreased over 6% in the last 7 years, while employer coverage has increased over 3% during the same period.
In a matter of two weeks, SIIA sent out a coalition letter to all 435 Members of Congress with 45 signatories, comprised of national, state and regional associations, employer groups and unions in opposition to the dialysis legislation.
Employer plans are covering more dialysis, not less. The kicker, the U.S. Department of Health & Human Services itself said that the Supreme Court did nothing to change the current MSPA protections.
To help counteract the fact that the dialysis providers had laid political groundwork for years in lobbying expenditures, SIIA immediately took an industry wide approach, and discussed the issues with employer
This was just the beginning of nearly 90 congressional meetings that SIIA held over the course of the next 4 months, encompassing House and Senate leadership, key committees, and individual Member staff. It became weekly planning calls, monthly coalition calls, and ongoing policy stakeholder meetings.
Slowly but surely, SIIA was able to change the course of the dialogue away from the dialysis providers misdirection with data, facts and impacts to self-insured plans. By November, we felt we had a good chance of ensuring that it would not become a provision in a year-end omnibus spending package, what amounts to a “Christmas Tree” bill of policy inclusions.
In a display of the process working the way it should, the CBO did its work in an unbiased way, uninfluenced by the misdirection and returned a score that estimated the proposed would cost the government $8 billion.


It was at that moment a key policy win came into play. The dialysis providers and their supporters had been advocating for months that their proposal would both protect patient and lead to up to $4 billion in savings to Medicare.
In general, such savings are important to congressional policymakers who are always looking for cost savings to pay for other policy programs. Supporters of the legislation were so confident in the strength of their misdirection, that the Congressional sponsors asked for a legislative “score” from the Congressional Budget Office (“CBO”).
Even more alarming, the CBO estimated the cost to employers of the legislation would be $42 billion due to the increased cost of healthcare and an increase in costs of pre-tax health benefits. This unbiased, data driven analysis by the CBO, was a fatal blow to the legislation, and one SIIA quickly amplified in communications with congressional members and their staffs.
And yet, the dialysis providers had one last trick up their sleeves. As end of the year omnibus language was being put together, SIIA, coalition partners, and even congressional staff became surprised to learn that dialysis providers were tweaking legislative language to bring down the cost and put it in to a last-minute deal. They did this behind closed doors, putting patient groups out in front with grassroots ads in Hill news outlets, and placing op-eds in D.C. and even Delaware, aiming to get to the President.
At this point, SIIA and its partners on the Hill doubled down on meetings and messaging.
One week later, on December 20th, omnibus language came out void of the special interest language put forward by the dialysis providers and their Hill allies. Common sense and good policy prevailed. Considering the time, funding and effort put in over years by the dialysis duopoly, this was a major win for employer-sponsored health, and self-insured plans specifically.
But our work isn’t over. SIIA fully expects the dialysis providers and their partners to introduce revised legislation in the next Congress, particularly considering that Senate sponsor, Sen. Cassidy (R-LA), will be the next ranking member of the Senate Health Committee.
When it happens, SIIA and coalition partners will be more prepared to fight back. This is a policy and political campaign that should be based on facts and market realities.
Unfortunately, it is being subjected to the funding and misdirection of the dialysis provider duopoly. It’s one that SIIA will continue to be at the forefront of – based on data, common sense, and member engagement. We want to shed light on the dialysis industry, through regular order, hearings and transparency. SIIA will continue to take an important lead on this and other policy issues on behalf of our members.



WhileThe No Surprises Act—which went into effect in January 2022—may not have an initial impact on health care captives, the ramifications of the act still need to be carefully considered.

“The primary beneficiaries of the legislation are individuals,” said Matthew Drakeley, vice president, specialty markets at QBE. “They were getting the surprise billing, some getting a five-figure bill from a provider. If this protects consumers going forward, that’s a benefit.”
Because many of those with health insurance get coverage through their employer, the employer has a managerial obligation, “to make sure their third-party administrator is capable of handling the responsibilities for the payer under the No Surprises Act,” Drakeley explained.
The hidden issue for payers and captives is the longer-term impact of the legislation. “Hospitals are already struggling with the increase of general inflation and labor costs in order to run their operations and provide services,” he said.
Over the last 30 years hospitals have had to find new ways to obtain revenue consistent with their expenses, Drakeley explained. The No Surprises Act, however, reduces a revenue source they had counted on to run their business. When balance billing gets reduced, hospitals’ revenues are also reduced.
“Coupling that with their increased expenses, it will probably impact hospitals that are renegotiating their contracts with networks, by raising their overall reimbursement,” he said. “So, we may see an increase in medical inflation as a result.”
When you add the general inflation in the economy, “that’s where it will impact payers and in some cases captives because both have a responsibility for paying claim liability,” Drakeley said.
“It’s an interesting time for captives, because the captive participant, the employer, is a certain type of employer who wants to gain as much control over their health care financing as they have of their overall balance sheet,” said Phil Holowka, chief operating officer at Complete Captive Management Services LLC. “That’s the common bond amongst captive members.”
This is also what is exciting for the captive community, “because they are not necessarily shopping for the lowest cost insurance policy, they are looking for a longterm solution to their financing risk,” he explained.
For
What will emerge from this, Holowka said, is the necessity for employers to look for resolutions, “which may not include accessing managed care.”
Captives, he said, can collaborate and hire service providers to spotlight opportunities for savings, such as using lower cost hospital facilities. The service provider, he said, “can notify employers that, within a 20-mile radius, these are the top five hospitals you should encourage employees to visit.”
He added that while the NSA will likely be a short-term disruption, “ultimately, in three to five years when these managed care contracts are renegotiated, the only loss would be an opportunity savings cost that was lost,” if knowledge about lower cost facilities wasn’t passed on to employees, as well as providing incentives to utilize them, Holowka said.
The effect of the NSA , he said, will be increased transparency for health plans. “Transparency is key, because it gives employer groups the power to understand their spend and reduce spend through cost containment programs,” he said. “As a captive that works with self-insured groups, we support that, because transparency drives knowledge.”
The initial impact is that more and more groups and companies are wanting to self-insure, said Chris Zirke, general counsel at Roundstone.
he said.
These are employers that typically had fully insured health plans and are paying one large monthly premium, but with very little understanding of where their claim is going, he said.

The situation is leading more people to selfinsurance as a solution, “because you don’t get a lot of transparency when you’re fully insured,”
“So, on a high level we’re seeing more groups wanting to self-insure because of the transparency in understanding their claims spend.”
Skyrocketing prices. Administrative challenges. Shock claims. Aging workforces. At Amwins Group Benefits, we’re here to answer the call. We provide solutions to help your clients manage costs and take care of their people. So whether you need a partner for the day-to-day or a problem solver for the complex, our goal is simple: whenever you think of group benefits, you think of us.
The benefits landscape is broad and complex.
Since being a captive member is more about controlling costs in the long term, “What will come out of this is, employers will look for better solutions, which may not include accessing managed care,” he said.
A captive attracts an employer who is generally more sophisticated and will have a desire to know everything they are paying for regarding health insurance, he said, “So, I would suggest that the no surprises act is really going to accelerate an employer that participates in a captive to rethink their membership in a managed care program.”
Part of the appeal of the captive solution is that these employers are not on their own. In a group captive, a number of parties work together. “In the captive we are the captive manager and the managing general underwriter, and there is also the third-party administrator,” Zirke said.
NSA requirements apply to all healthcare insurers, whether fully or self-insured. “When you’re fully insured these requirements fall upon the insurance carrier, but you are your own insurance carrier,” he said. “The benefits of NSA impact self-insured groups because of transparency, so you understand your spend,” he said.
Zirke added that most of their captive participants have health care advisors or brokers running their captive. “We as a captive get together with them a couple of times a year to discuss various topics,” he said. “We’re meeting
in January, and we’ll have a meeting in May, so we are in constant communication with these groups’ advisors.”
The No Surprises Act went into effect Jan. 1, 2022. It was written to protect consumers from unexpected out-of-network medicals bills and balance billing, often associated with emergency hospital visits. The Peterson Kaiser Family Foundation Health System Tracker states that of those with large employer coverage, 18 percent of all emergency visits and 16 percent of in-network hospital stays resulted in at least one out-of-network charge.
“The NSA applies to most private health plans offered by employers, as well as non-group health insurance policies offered through and outside of the marketplace. The new law contains other related provisions, including a requirement for health plans to keep network provider directories up to date,” according to Peterson KFF.
“This is a big topic these days for a number of different reasons,” said Chris Zirke, general counsel at Roundstone. “Part of it is the implications that Congress isn’t always clear, and part of it is that we’re all figuring it out and deadlines change, so it’s really interesting.”
Transparency rules help individuals and groups by reducing balance billing, he said. The reason this happens is that it isn’t always clear who is in and who is out of network, “especially at a hospital,” he said. A hospital, for example, “might be in network, but your doctor or provider might not, so part of it is covered by insurance and part is not,” Zirke explained. “You, as a patient might receive a large bill, which is a surprise because you thought it would be covered by insurance.”
This also happens in non-emergency situations, when patients at in-network hospitals or other facilities receive care from supplementary providers, such as anesthesiologists, who are not in-network and not chosen by the patient.
The No Surprises Act was put in place to end this practice, which is a direct benefit to the consumer. “There are also several other pieces to the NSA, part of which is a drug benefit to consumers. We support this because it drives down claims,” Zirke said. “Part of the benefit is to the employer, which is what makes up our captives. It all goes to help reduce claims spend and we help groups understand that.”
Zirke noted that what captives can be doing now is educating themselves about the act and planning how to cover all their bases.
Caroline McDonald is an award-winning journalist who has reported on a wide variety of insurance topics. Her beat has included in-depth coverage of risk management and captives.
A first-of-its-kind healthcare SuperApp for self-funded plan sponsors that helps members make better decisions around quality medical care delivery, so everyone wins.
The only self-funded healthcare engagement platform of its kind.

Hercules Health rewards habitual app utilization by giving cash incentives earned through intelligent healthcare shopping tied to quality and cost. More app use equals more savings for members and plan sponsors alike.


Hercules Health delivers best-in-class price transparency that is fully compliant with the Transparency in Coverage (TiC) and the No Surprises Act (NSA) rules and regulations.
 Written By Andrew Silverio, Esq.
Written By Andrew Silverio, Esq.
TheTCOVID-19 pandemic has given rise to many practical and regulatory challenges for self-funded plans and those that serve them. Most of these regulatory changes create important protections for plan participants but create significant burdens and potential exposure for plans – this includes significant expansions to COBRA rights under the American Rescue Plan Act of 2021, vaccine and testing mandates under the FFCRA and CARES Act, and the extension of various plan deadlines relating to claim submission, appeals, enrollment, and COBRA.
There is an important allowance in the CARES Act which benefits both plans and participants, however – under this, high deductible health plans (HDHPs) may provide benefits for telehealth services without application of any cost-sharing and without regard to whether any deductible has been met without impacting the plans’ ability to be paired with a health savings account (HSA).
At Vālenz® Health, our culture of innovation demands taking risks, making smart decisions and occasionally spilling a little milk. And when those mistakes happen, we quickly adapt and move forward with even better solutions.
That’s why our customers choose and stay with Valenz. We might spill some milk together, but in the process, we build a partnership based on trust, collaboration and results.
It’s our culture that makes us different, which is why we wear it on our sleeves.

Without this allowance, an HDHP providing any “first-dollar” coverage for non-preventive services would destroy the plan’s HSA compatibility, having serious tax consequences for all participants utilizing the HSA. This allowance was set to expire at the end of 2022; however, the passage of the Consolidated Omnibus Appropriations Act (2023) extends it through the end of 2024.
This means that HDHPs using HSAs may (but are not required to) continue to offer first-dollar coverage for telehealth and telemedicine services, whether preventive, through the end of plan years beginning on or before December 31, 2024.

It's important to note, however, that this relief does not include an extension of a waiver that currently allows providers to prescribe controlled substances via telehealth for substance abuse treatment. Because of this, most telehealth providers will default back to existing regulations which severely limit their ability to prescribe controlled substances for patients they haven’t treated in person.
The need for this relief is attributable to the severe restrictions imposed on HDHPs by the regulations governing HSAs. In order to utilize an HSA, an individual must be covered under an HDHP which complies with strict limitations, most notably that the plan applies at least a minimum required deductible to almost all non-preventive services
($1,500 for individual coverage in 2023).
Additionally, an individual using an HSA must have no other health coverage besides that HDHP. These requirements in tandem severely limit HDHPs’ ability to create steerage within the plan benefit structure, and thus their ability to utilize many popular cost-containment techniques.
For example, an HDHP cannot exempt certain high-cost non-preventive drugs from its deductible to steer individuals toward a specialty management program without bumping up against the “first-dollar” coverage requirement, while it also can’t create parallel coverage for those drugs outside the plan without bumping up against the “other coverage” problem.
These challenges are the major trade-off HDHP sponsors make in return for the tax benefits of making an HSA available.
Join industry leaders at SIIA’s Price Transparency Collaboration Forum February 27th and Tuesday, February 28th the Kansas City Marriott for a unique opportunity to take a deep dive into the various new and ongoing federal price transparency regulations and their impact on self-insured health plans.
The Forum will provide insights from key government regulators, explore best practices, and discuss collaboration initiatives to help bolster compliance, understanding and opportunities between industry executives and partners from across the self-insured space.
From the Transparency in Coverage regulations to the No Surprises Act, this Forum will provide a chance to gain in-depth knowledge about what these evolving rules and regulations mean for your business and clients, from strategy to implementation.

Networking and Program highlights include:
Help support the Self-Insurance Political Action Committee (SIPAC) and compete against colleagues and other SIIA members during a fun and interactive ax throwing competition and reception. Network with other industry participants, throw axes, and support our industry’s political advocacy activities as we begin the 2024 election cycle.
know analysis on current federal price transparency activities, ranging from the Hospital Price Transparency and Transparency in Coverage Rules to the ongoing implementation of the No Surprises Act.
PANELISTS:
Chris Condeluci
Washington Counsel
Join other younger attendees for an on informal “on your own” afterdinner networking event.
Self-Insurance Institute of America, Inc. (SIIA)
Ryan Work
Senior Vice President, Government Relations

Price Transparency: Policy & Regulatory Update
SIIA’s Government Relations Team will provide insights and need to
Self-Insurance Institute of America, Inc. (SIIA)

Key federal agency regulators will discuss details on federal transparency rules, in addition to insights into future guidance and implementation recommendations.
PANELISTS (Invited):
Beth Baum
Senior Advisor
U.S. Department of Labor
Deborah Bryant
Special Advisor for the Consumer Support Group, Center for Consumer Information and Insurance Oversight (CCIIO) Center for Medicare & Medicaid Services
Lindsey Murtagh
Director, Market-Wide Regulation Division, Center for Consumer Information and Insurance Oversight (CCIIO)
Centers for Medicare & Medicaid Services
Price Transparency
Collaboration: Working with TPAs, Broker, Advisors & Stops Loss Carriers

Price transparency mandates and reporting requirements mean an increasing need for collaboration from entities working on behalf of a self-insured plan. This panel will explore best practices in working across entities in compiling, reporting, and submitting planrelated requirements in the price transparency space and assist in navigating roles and responsibilities.
PANELISTS:
Dennis Charland
Senior Vice President Zelis
Josh Silverman
Chief Transformation Officer
Allied Benefits
Kelly Wage
VP, Consumer Experience and Market Solutions
Blue Cross Blue Shield of South Carolina
Taking Advantage of Pricing
Transparency for a Healthcare Consumer-Minded Member Strategy
Federal Price Transparency has unlocked more consumer information than ever before, which can potentially transform the delivery of healthcare services by allowing patients to proactively make informed, cost-conscious
decisions about their health. What can the self-insured industry do to educate patients, and effectively access and utilize service information and cost before receiving care? Further, our panelists will explore how to handle the claims once the care is received and what can be done to control costs on behalf of the member and self-insured plan.
PANELISTS:
Katy Brant President
6 Degrees Health
Bill Kampine
Co-founder & Chief Innovation Officer Healthcare Blue BookData Accessibility & Price
Transparency: Understanding Exposure
A legal and industry take on data accessibility issues, exposure, and other issues related to NSA and TiC Rules, including real-world legal and contract issues faced by plan service providers.
PANELISTS (Invited):
Dawn Cornelis
Co-Founder
ClaimInformatics
Nick Welle Partner
The Risk Strategies National Healthcare Practice provides specialized expertise and solutions to the healthcare industry across all aspects of the business - Employee Benefits, Managed Care Risk, Reinsurance and Property, Casualty and Liability.

By bringing together one of the largest teams of dedicated healthcare insurance and reinsurance professionals operating across the country, Risk Strategies offers its healthcare clients a focused, integrated and responsive liability and risk management service that is best-in-class.
Risk.
Foley & Lardner, LLP risk-strategies.com/healthcare
With one year since plans started implementing NSA programs and the Open Negotiation and IDR process began, this session explores what industry participants need to know, lessons learned, and how to tackle the open negotiation and IDR/ arbitration process.
PANELISTS:
Tim McConville
Managing Attorney
ClearHealth Strategies
Troy Sisum
Chief Legal Officer
Imagine 360
A Fair Price: Getting to & Understanding
Hospital & Provider Pricing
Federal price transparency often hinges on provider and hospital pricing, billing and QPA calculations. What do self-insured entities need to know about evolving hospital billing practices, what are key lessons learned, and how can you use hospital data to assist in surprise billing and beyond.
PANELISTS:
Douglas Aldeen, Esq. Attorney at Law
David Cardelle Chief Strategy Officer
Advanced Medical Strategies (AMS)

Air Ambulance: The Other Side of Surprise Billing
An often-overlooked piece of the No Surprises Act, air ambulance claims are increasingly costly for self-insured plans. This panel will delve into recent air ambulance claim trends, and what self-insured entities need to
understand about the unique treatment of it under the NSA.
PANELISTS:
Jeff Frazier
Sentinel Air Medical Alliance
Jennifer Hill
AVP, Complex Claims
Lockton Companies
Price Transparency Town Hall
This closing interactive session will allow participants to ask questions from the day’s topics, talk about experiences, challenges and opportunities, and provide a forum on all things healthcare transparency.
For more information including registration and sponsorship opportunities, visit www.siia.org.


SIIA Diamond, Gold, and Silver member companies are leaders in the self-insurance/captive insurance marketplace. Provided below are news highlights from these upgraded members. News items should be submitted to membernews@siia.org
All submissions are subject to editing for brevity. Information about upgraded memberships can be accessed online at www.siia.org.
If you would like to learn more about the benefits of SIIA’s premium memberships, please contact Jennifer Ivy at jivy@siia.org
You want unparalleled customer service. Employers need the right stop loss coverage. At Swiss Re Corporate Solutions, we deliver both. We combine cutting-edge risk knowledge with tech-driven solutions and a commitment to put our customers first. We make it easy to do business with us and relentlessly go above and beyond to make stop loss simpler, smarter, faster and better. We’re addressing industry inefficiencies and customer pain points, moving the industry forward – rethinking employer stop loss coverage with you in mind. corporatesolutions.swissre.com/esl
Portsmouth, NH – TALON, an industry leader in providing groundbreaking healthcare technology solutions, announced that Naresh Parmar has joined its growing team as Senior Vice President, Product.
With three decades of experience in product and portfolio management, global delivery execution, client services, and the development and implementation of robust, data-driven technology solutions across verticals, Parmar comes to TALON from Data Axle, where he served as Senior VP of Digital Technology.
While there, he led digital marketing technology solutions, including cloud technologies and data analytics, for local and global clients in the healthcare, finance, retail, automotive, travel, and hospitality industries. Before that, he spent seven years as Vice President, Solutions Architecture and Delivery at Epsilon.
“Naresh is a phenomenal addition to the TALON team. His reputation and proven successes in creating value for end-users and stakeholders by leveraging technology speak true to his exceptional capabilities,” said TALON Co-Founder, President, and CEO Mark Galvin. “As the healthcare ecosystem rapidly
evolves in the age of total pricing transparency, and TALON continues to seamlessly meet the needs of that advancing ecosystem with innovative, scalable technology solutions, Naresh’s expertise will be paramount.”
Parmar said in a statement.
Portsmouth, NH – TALON, a leader in providing innovative technology solutions for the swiftly evolving healthcare industry, announced that Sean Signore has joined its growing team as Vice President of Training and Certification.
Signore is a skilled learning strategist with more than 16 years of experience in learning and development (L&D) program management. His proven track record of leading teams and functions across regional, divisional, and international operations includes expertise in overhauling L&D strategies to bolster organizational efficacy, employee development, and workflow coordination; aligning organization direction with content strategies and staff training; as well as a deep proficiency with process consultant coaching models.
Signore comes to TALON from Teknova, where he served as Training and Development Manager and was responsible for conducting needs analyses for strategic learning infrastructure from a risk-based perspective, as well as designing and facilitating in-person learning interventions to engage leadership and improve manufacturing goals.
“TALON has a stellar reputation in the healthcare technology space, and I’m thrilled to join their rapidly expanding team,” Signore said in statement. “I’m eager to dig in and, together with my exceptionally talented colleagues, continue to push the envelope and supply the
“The healthcare industry has entered a new reality—a participant-driven marketplace.
TALON is at the forefront of providing the technology and tools necessary to be successful in this new era,”
“I’m very excited to join such a talented and dynamic team.”
groundbreaking technology solutions that the modern healthcare industry demands.”
TALON’s mission is to educate, empower, and incentivize the American healthcare consumer to meaningfully reduce costs and create a healthier ecosystem. We’ve built the ultimate suite of software services designed to fulfill the requirements of the Transparency in Coverage Rule and No Surprises Act. Simply put, TALON protects healthcare stakeholders from overpaying for
care while enabling seamless integration into the Payer’s existing architecture, all without disruption or distraction. Our tools create free-market dynamics, starting with our ability to ensure full compliance with all mandates and extending through our consumer-driven MyMedicalShopper platform. Learn more at www.talonhealthtech.com.
BLACKWELL CAPTIVE SOLUTIONS PARTNERS WITH BRELLA

Chicago, IL – According to a Kaiser Family Foundation poll, approximately 50 million adults – roughly 1 in 5 – are paying off bills for their own care or a family member’s care through an installment plan with a hospital or other provider and beset by a health care system that is systematically pushing patients into debt on a mass scale.

To ease some of the financial burden of out-of-pocket medical bills for members, Blackwell Captive Solutions has strategically partnered with Brella to help clients supercharge their health benefit strategies.
Blackwell clients now have access to Brella’s supplemental health insurance product to ease the financial impact of unexpected medical expenses. One Brella plan covers over 13,000 separate conditions. Brella provides employers with 100% paperless, same-day plan implementation, and enables members to file claims in minutes and get paid in just 72 hours after approval. Their state-of-the-art mobile app and member portal make the claim filing and payment processes simpler and faster, and Brella plans are guaranteed issue with no medical underwriting ever.
“Whether a team is remote, onsite or hybrid is less important than enhancing the employee experience and shifting the focus to a diverse and heightened benefit portfolio, customized to each employee and unconfined, to be noticeable from competition. Thus, we are excited to partner with Brella and squarely deliver on lessening the
financial burden of our health care system for our clients and their members,” said Kari L. Niblack, President, Blackwell Captive Solutions. “Together, we move! Let’s see what Brella and Blackwell can do for you and your employees.”
Headquartered in Chicago, Blackwell Captive Solutions is a medical stop loss captive that differentiates by delivering essential stability with desired flexibility via access to cutting-edge health and well-being solutions for our clients. We’ve proven


Ringmaster Technologies’ pharmacy consulting platform presented by its wholly owned subsidiary, “Ringmaster Rx”, is a huge win for Brokers, TPAs, and PBMs (pharmacy benefits managers). Its cloudbased data warehouse integrated with a RFP workflow process gives clients the ability to:
• Solicit, Compare and Award PBM Contracts and Programs
• Perform contract reconciliations & audits on contract performance
• Deliver sophisticated analytics and generate value added reports
• Customize their own panel of preferred PBM’s
• Efficiently manage cost for their employer groups

that combining employers’ buying power with tailoring freedom maximizes the impact of self-insurance and reduces market volatility associated with the ultimate cost of healthcare benefit delivery to employees. Visit www.blackwellcaptive.com
NEW YORK -- Marpai, Inc., an AI-technology company transforming self-funded employer health plans, introduces Marpai Chronic Condition Management to improve the care journey of members with chronic conditions like heart disease, respiratory disease, diabetes, kidney disease and mental health.

This is the latest addition to Marpai's Clinical Services Ecosystem – proven, clinical care solutions, backed by outcome and quality data, delivering specialized strategies and support to manage costly conditions.
Leveraging the most advanced artificial intelligence, Marpai's proprietary clinical matchmaking platform identifies at-risk health plan members where a clinical intervention can make a meaningful difference and connects them to an appropriate solution in the Clinical Services Ecosystem. By addressing costly conditions early and appropriately, Marpai aims to create healthier lives and reduce health
plan costs for employers.
According to the Centers for Disease Control and Prevention (CDC), in 2018 51.8% (129 million) of U.S. adults have been diagnosed with at least 1 of 10 selected chronic conditions: 24.6% (61 million) with one chronic condition and 27.2% (68 million) with two or more chronic conditions.
It is estimated that 86% of healthcare costs are attributable to chronic disease which makes it a formidable challenge for employer health plans, especially self-funded health plans.
"Chronic conditions are highly prevalent across our member populations and are extremely costly. We are delighted to introduce this service to address
We study it, research it, speak on it, share insights on it and pioneer new ways to manage it. With underwriters who have many years of experience as well as deep specialty and technical expertise, we’re proud to be acknowledged as experts in understanding risk. We continually search for fresh approaches, respond proactively to market changes, and bring new flexibility to our products. Our clients have been benefiting from our expertise for over 45 years. To be prepared for what tomorrow brings, contact us for all your medical stop loss and organ transplant needs.

these issues. Our team of medical experts use evidence-based tools to help members take the best care journey. Their efforts have proven to reduce ER visits, hospital stays and medication costs which significantly helps reduce plan costs for employers," says Marpai's Chief Executive Officer, Edmundo Gonzalez.
Marpai Chronic Condition Management is part of the Marpai Cares offering which is available to all health plan members under Marpai's administration. Marpai's AI-powered clinical matchmaking system proactively identifies at-risk members where a clinical intervention could make a meaningful difference within 24 months, and matches them to a clinical solution in its Clinical Services Ecosystem.
The Ecosystem consists of clinical solutions rigorously vetted by Marpai data scientists and clinicians, and supported by valid outcome and quality data. Marpai aims to add 15 more Clinical Health Partners by the end of 2023.
About Marpai, Inc.
Marpai is a technology company bringing AI-powered health plan administration and services to employers that directly pay for employee
health benefits (self-funded employer health plans). Primarily competing in the $22 billion TPA (Third Party Administrator) sector representing over $1 trillion in annual claims, Marpai is committed to delivering the healthiest member population with the greatest cost efficiency within the health plan budget. Marpai leverages AI and big data to proactively implement early clinical interventions to improve near-term outcomes, fill gaps in annual care, and guide members to high-value in-network providers and pharmacy solutions. Operating nationwide, Marpai offers access to provider networks including Aetna and Cigna and delivers all standard TPA services. Visit www.marpaihealth.com
The right pharmacy management solution can assist employers in optimizing costs and health outcomes. The right TPA can help clients connect the dots between clinical data, member utilization and plan spend.
CHAIRWOMAN OF THE BOARD*
Elizabeth Midtlien
Vice President, Emerging Markets
AmeriHealth Administrators, Inc.
Bloomington, MN
CHAIRMAN ELECT & TREASURER AND CORPORATE SECRETARY *
John Capasso
President & CEO
Captive Planning Associates, LLC
Marlton, NJ
DIRECTOR
Stacy Borans
Founder/Chief Medical Officer
Advanced Medical Strategies
Lynnfield, MA
DIRECTOR
Matt Kirk President
The Benecon Group
Lititz, PA
DIRECTOR
Mark Combs
CEO/President
Self-Insured Reporting
Greenville, SC
DIRECTOR
Shaun L. Peterson
VP, Stop Loss
Voya Financial
Minneapolis, MN
DIRECTOR
Amy Gasbarro
Chief Operating Officer
Vālenz
Phoenix, AZ
DIRECTOR
Adam Russo CEO
The Phia Group, LLC
Canton, MA
DIRECTOR
Deborah Hodges President & CEO
Health Plans, Inc.
Westborough, MA
Captive Insurance Committee
Jeffrey Fitzgerald
Vice President
Innovative Captive Strategies
Waukee, IA
Future Leaders Committee
Erin Duffy
Director of Business Development
Imagine360 Wayne, PA
Price Transparency Committee
Christine Cooper CEO
aequum, LLC
Cleveland, OH
Captive Insurance Advocacy
Task Force
Jeffrey K. Simpson Partner
Womble Bond Dickinson (US) LLP
Wilmington, DE
Workers’ Compensation Committee
Shelly Brotzge
Regional Underwriter, Group Self Insurance
Midwest Employers Casualty
Chesterfield, MO
CHAIRMAN
Nigel Wallbank
Preisdent
Leadenhall, LLC
Ocala, FL
PRESIDENT
Daniél C. Kimlinger, Ph.D.
CEO
MINES and Associates
Littleton, CO
DIRECTORS
Freda Bacon
Administrator
AL Self-Insured Workers' Comp Fund
Birmingham, AL
Les Boughner
Chairman
Advantage Insurance Management (USA) LLC
Charleston, SC
Alex Giordano
Chief Executive Officer
Hudson Atlantic Benefits
Bellmore, NY
Virginia Johnson
Strategic Account Director
Verisk/ISO Claims Partners
Charlotte, NC
* Also serves as Director























Todd Archer President Concierge Third Party Administrator Bartlesville, OK

Robert Heintz President Edge Insurance Group
Grandville, MI

Michael Kelly Vice President HealthCheck360 Dubuque, IA
Linda Maxson Events Manager IQVIA Wayne, PA
Nancy Fleming Marketing Director Serve You Rx Milwaukee, WI
Julia Paphitis Vice President Sales and Business Development CEN Highland Park, IL













Catastrophic claims can arise unexpectedly. If the plan has the right Stop Loss protection in place, focus can remain on achieving business goals and welcoming Nadia back when it’s time. When you work with the experts at HM Insurance Group, you can have confidence that the claims will be paid. Find more on hmig.com
