Accident
& Health InsuranceWe’ll focus on risk, so you can take care of

Accident
& Health InsuranceWe’ll focus on risk, so you can take care of
Self-insuring your healthcare benefits can open up new possibilities for your business — affording you greater flexibility in how you manage your healthcare spend. Trust the expert team at QBE to tailor a solution that meets your unique needs.

We offer a range of products for protecting your team and assets:
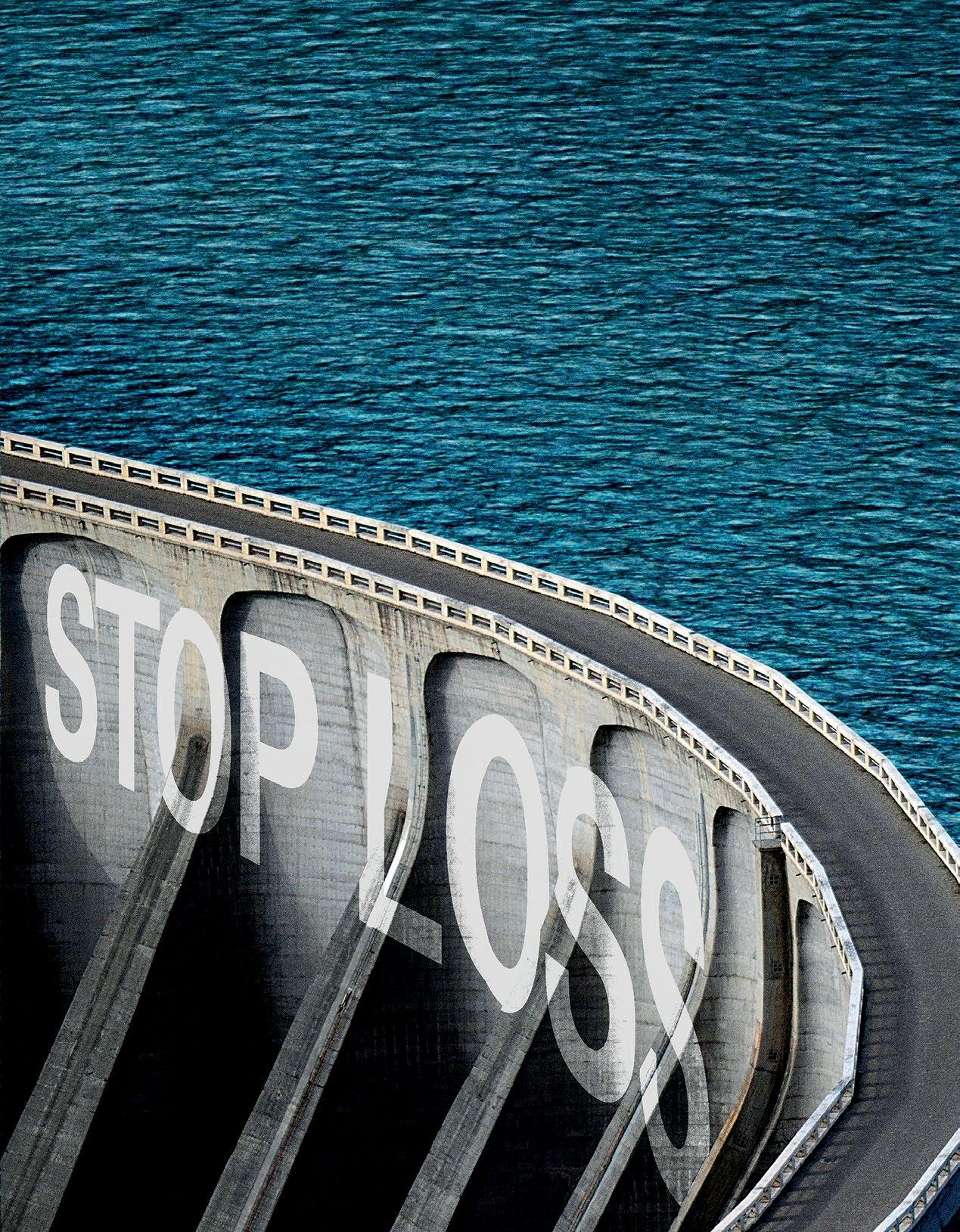
• Medical Stop Loss
• Captive Medical Stop Loss

• Organ Transplant
• Special Risk Accident
We’ll find the right answers together, so no matter what happens next, you can stay focused on your future.
FEATURES
4 EMPLOYERS PRIORITIZE BEHAVIORAL HEALTH
By Laura Carabello30 STEPPING UP CYBERSECURITY FROM TREATING EMAILS WITH CAUTION TO ENGAGING OUTSIDE EXPERTISE, ERECTING GUARDRAILS HAS BECOME NECESSARY FOR SELF-INSURED PLANS
 By Bruce Shutan
By Bruce Shutan
38 INFLATION COSTS IMPACTING CAPTIVE INSURANCE
45 ACA, HIPAA AND FEDERAL HEALTH BENEFIT MANDATES THE AFFORDABLE CARE ACT (ACA), THE HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT OF 1996 (HIPAA) AND OTHER FEDERAL HEALTH BENEFIT MANDATES
51 GENE AND CELL THERAPY: WHERE COMPASSION AND COST COLLIDE
55 NEWS FROM SIIA MEMBERS
PUBLISHING DIRECTOR Bryan Irland, SENIOR EDITOR Gretchen Grote, CONTRIBUTING EDITORS Mike Ferguson and Ryan Work, DIRECTOR OF ADVERTISING Shane Byars, EDITORIAL ADVISOR Bruce Shutan, CEO/Chairman, Erica M. Massey, CFO, Grace Chen

With the glare of the pandemic in the rear-view mirror, employers are re-energizing their efforts to improve the state of employee mental health.
While issues associated with isolation and loneliness exacerbated by COVID-19 still persists, the significant impact of anxiety, depression, substance use disorders (SUDs), financial stress, workplace environment and other looming crises all impact well-being and productivity at work.
Peter Robinson, managing principal, EPIC Reinsurance, shares this perspective, “This is a very timely topic and in reaching out
to various insurers and health plans, I was amazed at the priority this is being given. The impact of behavioral health (BH) on overall morbidity and related health costs is clear. Nearly every health care leader I spoke with referred to BH as a health emergency.”
Indeed, BH might well be an urgent priority given this statistic from the Substance Abuse and Mental Health Services Administration (SAMHSA): one in five adults in the U.S. have a clinically significant mental health or SUD. Furthermore, the prevalence and severity of mental health conditions among children and teens has increased sharply.
“Employers are increasing their BH offerings to employees,” says Deb Adler, CEO, Navigator Healthcare Inc. “This is based upon employers recognizing the importance of their employees’ mental health for productivity, retention, cost savings, and overall health outcomes.”

She cites the factors driving this focus: 1) Mental Healthcare/SUD which are typically the number 5 medical cost for employers, and 2) Anxiety and depression which increased by 25% during the pandemic, according to the World Health Organization.
The National Institute on Alcohol Abuse and Alcoholism found that alcohol consumption increased by 39% and binge drinking increased by 30%.
“The cost of SUD, anxiety and depression and children’s needs for mental health and/or autism services rank very high as increasing the employer’s medical costs the most, year over year,” continues Adler. “Stress and anxiety from meeting either your own personal needs or your family’s needs often results in missed days from work or even being at work but not truly engaged, known as presenteeism.”
Unfortunately, many people fail to receive treatment due in part to the long-standing shortage of BH providers. One indicator of the gravity of this problem is the newest CDC report on suicide which is now ranked
as the second leading cause of death in people aged 10–34 and the fifth in people aged 35–54.
Jakki Lynch RN, CCM, CMAS CCFA. director cost containment, Sequoia Reinsurance Services, emphasizes that BH risk exposure underscores the need for risk mitigation interventions and that these issues have long been a concern of health benefits managers.
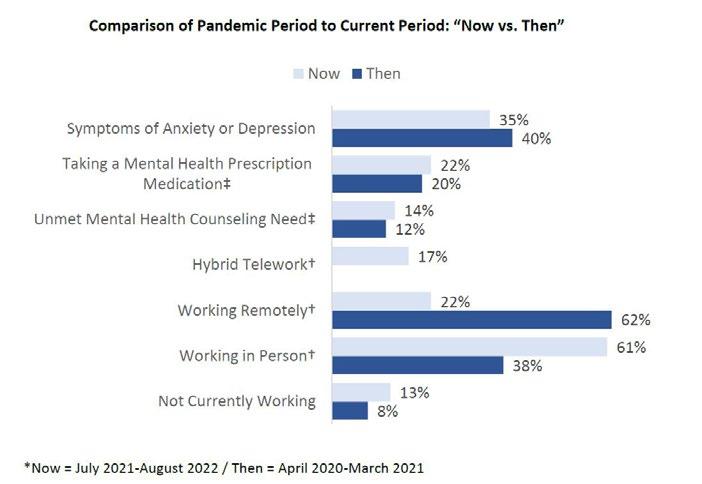
She points out that BH and substance use remain elevated three years after the onset of the COVID-19 pandemic, according to a recent Kaiser Family Foundation/CNN survey. KFF
performed an analysis of U.S. Census Bureau, Household Pulse Survey, 2020-2023 showing that more than 30% of surveyed adults reported symptoms of anxiety and depression, up from 11% in 2019.
“The key message for health plans is abundantly clear,” says Lynch. “The growing mental health crisis places an increased need for more access


In addition to claims and benefits administration, we offer pharmacy benefit management, health and wellness programs and stop-loss insurance, all backed by a dedicated in-house customer support team.
to treatment, and a proactive cost management approach to mitigate the associated BH service expenditures. With the influx in behavioral claim volume, the need for claim payment integrity is paramount for payers as experience shows that BH treatment claims are frequently not supported by the care that was rendered.”
America’s Health Rankings 2022 Annual Report shows that the prevalence of frequent mental distress increased 11% among adults between 2020 and 2021. This is alarming since employees with unresolved depression may experience a reduction in productivity, which may also affect their employers’ profitability. Conversely, a 2019 study from Oxford University found that happy workers are 13% more productive.
There is rising, widespread consensus regarding the need for behavioral health solutions since the advent of COVID. Julie Mueller, president & CEO, Custom Design Benefits reports that within their own book of business, they saw mental health claim costs increase from 3.6% in 2018 to almost 10% in 2022.

“Mental health costs have increased from about $23 PEPM to almost $39 PEPM during this same period,” says Mueller. “It’s obvious that employees and their employers need affordable and cost-effective solutions for mental
health care. However, most of the mental health claims that are coming through our clients’ plans are only treating the symptoms via medication vs. addressing the root cause of the mental health need.”
She suggests that the best solution is one that offers a variety of ways for assistance and meets the patient where they are, adding, “Crisis intervention, virtual visits with a therapist, in-person visits, text therapy, anonymous virtual group therapy sessions, videos and other digital resources can all play a role depending on what the patient needs and where they are in their journey to improve their well-being.”
Lynch cites a new JAMA study showing SUDs cost employersponsored health plans about $35.3 billion per year.
“According to a recent report from NPR, an insurance company received an inpatient rehabilitation claim for the treatment of SUD totaling $660K for 7 months of care and unfortunately, the patient ultimately expired from an overdose,” she continues.
“The three most common types of BH billing errors involve documentation, the number of units billed and plan benefit policy violations,” adds Lynch, citing a recent report from the Department of Health and Human Services’ Office of Inspector General.
“An example of incorrect billing from their report includes providers who billed for both a facility fee and a telehealth service. Two providers—a psychiatrist and psychologist—billed for both a facility fee and a telehealth service for more than 90% of their visits, amounting to nearly 4,000 visits each. The combined duplicate facility fees and telehealth services totaled approximately $1.1 million.”
She describes a recent high-dollar inpatient services claim for substance abuse treatment that was reviewed by her payment integrity team and identified $23,000 (19%) of total contract payable charges of $121,000 -- erroneously submitted from errors involving the number of units billed as the member did not receive the reported hours of treatment.
“Based on the claim payment integrity review, the treatment facility agreed these charges were not payable,” says Lynch. “Plans can successfully implement a comprehensive payment integrity program to mitigate significant risk for mental health encounters and treatment programs.”
Adler advises that the best practice for employers is to provide mental health services at no cost-share for the employees. “This ensures access and the right level of engagement with the high-quality mental health care offered, which leads to lower costs, better outcomes and higher employee satisfaction.”
Mueller explains that the behavioral health services that they administer for clients do not require a co-pay or any out-of-pocket expense.
“Our clients pay a monthly per-employee fee based on the number of


When choosing a provider network or tele-behavioral health solution, employers should be aware that the range of professionals who provide therapy may include different levels of training and capabilities, as described by the Mayo Clinic:
A psychiatrist is a physician — Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) — who specializes in mental health. This type of doctor may further specialize in areas such as child and adolescent, geriatric, or addiction psychiatry. This provider can identify and treat mental health conditions and A psychiatrist also can offer talk therapy, sometimes called psychotherapy. A psychologist is trained in psychology — a science that deals with thoughts, emotions and behaviors. Typically, a psychologist holds a doctoral degree, such as a Ph.D. or Psy.D. A psychologist can identify and treat many types of mental health conditions. This provider offers different types of talk therapy. In the U.S., most psychologists are not licensed to prescribe medicine. But they may work with another provider who can prescribe medicine if needed.
Less of everything that holds you back. More of everything that makes you great.
From locally-focused to national-scale programs, AmeriHealth Administrators offers a full spectrum of third-party administration and business process outsourcing services. Our scalable capabilities service many unique customers, including self-funded employers, Tribal nations, international travelers, and labor organizations.
We offer innovative solutions, insight, and expertise to help you manage your health plan and capabilities, control costs, and support employees’ health.
Visit amerihealth.com/tpa


A psychiatric mental health nurse (P.M.H.N.) is a registered nurse (R.N.) with training in mental health issues. A psychiatric mental health advanced-practice registered nurse (P.M.H.-A.P.R.N.) has at least a master’s degree in psychiatric mental health nursing. Other types of advanced-practice nurses who offer mental health services include a clinical nurse specialist (C.N.S.), a nurse practitioner (N.P.) and a nurse with a doctorate of nursing practice degree (D.N.P.). The services offered by mental health nurses depend on their education, level of training, experience, and state law. They can identify and treat mental illnesses. If state law allows, advanced-practice nurses can prescribe medicine.
A physician assistant (P.A.) practices medicine as a primary care provider or works together with a physician. Physician assistants can specialize in psychiatry and can identify and treat mental health conditions. They also can counsel on causes, treatments, and outlook.
A physician assistant can prescribe medicine.
Licensed clinical social worker
Look for a licensed clinical social worker (L.C.S.W.) with training and experience in mental health. A licensed clinical social worker must have a master’s degree in social work. Some have a doctorate in social work. Social workers offer assessment, counseling and a range of other services. What services they offer depends on their licensing and training. They are not licensed to prescribe medicines. But they may work with another provider who can prescribe medicine if needed.
Licensed professional counselor
Training required for a licensed professional counselor (L.P.C.), licensed clinical professional counselor (L.C.P.C.) or similar titles may vary by state, but most have at least a master’s degree with clinical experience. These licensed counselors identify mental health conditions and give counseling for a range of concerns. They are not licensed to prescribe medicine. But they may work with another provider who can prescribe medicine if needed.
Skyrocketing prices. Administrative challenges. Shock claims. Aging workforces. At Amwins Group Benefits, we’re here to answer the call. We provide solutions to help your clients manage costs and take care of their people. So whether you need a partner for the day-to-day or a problem solver for the complex, our goal is simple: whenever you think of group benefits, you think of us.
We help you win.
The benefits landscape is broad and complex.
A marriage and family therapist (M.F.T.) is trained in family and individual therapy. This type of therapist can help people to overcome family problems or issues in other relationships. They have at least a master’s degree. License and certificate requirements vary by state. Look for a licensed marriage and family therapist (L.M.F.T.). These therapists may work independently or in partnership with other professionals.

Employers should be cognizant of these medicines since they impact the drug benefit plan. Antidepressants are common prescription medications that can help treat depression and other conditions like anxiety and obsessive-compulsive disorder.
There are several types of antidepressants, and each individual should consult with a healthcare provider to find the best one for his/her condition.
Antidepressants were invented in the 1950’s and today, a new generation of drugs for depression is stirring excitement and transforming the way scientists and clinicians diagnose, treat and think about the illness. Antidepressants are one of the most frequently prescribed medications in the United States. The Cleveland Clinic advises antidepressants are simply one type of treatment for depression. While they can treat the symptoms of depression, they don’t always address its causes. This is why healthcare providers often recommend psychotherapy therapy in addition to depression medication.
One prescription digital therapeutic (DT) that is aimed at treating alcohol use disorder (AUD) was recently granted breakthrough device designation by the FDA.

While this suggests the regulatory agency believes the therapy has the potential to provide substantial improvement in patient care compared to existing therapies, not all mental health apps may be ready for prime time.
The demise of the two leading, well-funded companies tells a different story.

One company had a clearance for software as a medical device for mental health and may have offered a pathway toward improved access, remote diagnosis and monitoring of mental health conditions –even help to cure addiction.
But neither company was able to invest the money to carry out the necessary scientific research. While DT companies may be stumbling in 2023, industry observers remain hopeful that this approach will achieve scientific reality.

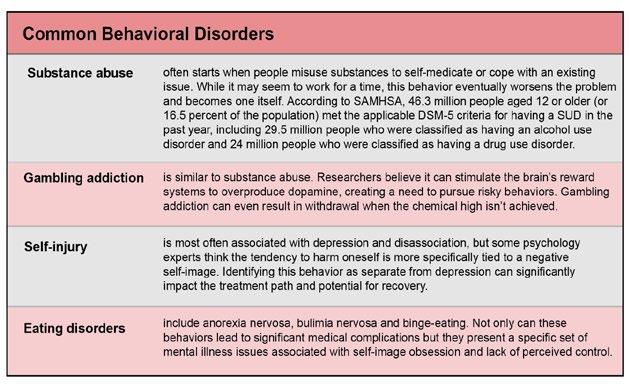
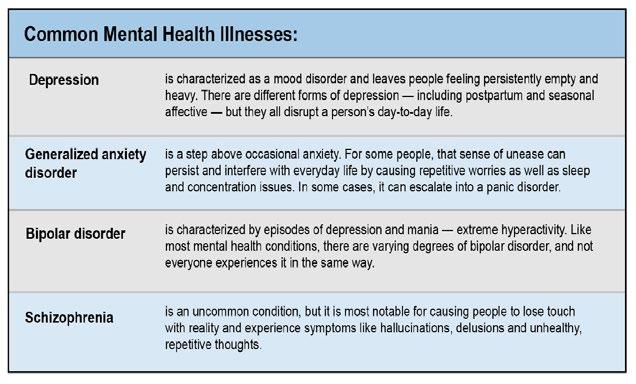
The terms “behavioral health” and “mental health” are often used interchangeably, but there are subtle differences and approaches to managing problems.
Behavioral Health as defined by the American Medical Association generally refers to SUD, life stressors and crises, and stress-related physical symptoms. The discipline examines how a person’s habits impact their overall physical and mental wellbeing and has more to do with the specific actions people take and how they respond in various scenarios.
Mental health as defined by The World Health Organization is “a state of wellbeing in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully and is able to make a contribution to his or her community.”
The term encompasses a number of factors, such as the individual’s biology, psychological condition and habits and has more to do with thoughts and feelings.
Negative behaviors don’t always accompany these mental health conditions. Most everyone with depression, for example, experiences sleep issues. But not everyone develops a behavioral disorder. When a distinct, regular behavior that goes beyond the scope of a typical mental illness begins to negatively affect someone, it becomes a disorder that typically requires more specific treatment.
Sources:
https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/ NSDUHFFR2017.pdf
https://wisqars.cdc.gov/data/lcd/home
https://www.samhsa.gov/data/report/2017-nsduh-annual-national-report
https://www.scientificamerican.com/article/how-the-brain-gets-addicted-togambling/
https://www.apa.org/monitor/2015/07-08/self-injury
https://www.mentalhealth.gov/what-to-look-for/mental-health-substance-usedisorders
https://www.nimh.nih.gov/health/publications/eating-disorders
Sources: Alvarado Parkway Institute. https://apibhs.com/2018/05/10/the-differencebetween-mental-and-behavioral-health
https://www.nimh.nih.gov/health/statistics/any-mood-disorder
https://www.nimh.nih.gov/health/topics/depression
https://www.nimh.nih.gov/health/topics/anxiety-disorders
https://www.nimh.nih.gov/health/topics/bipolar-disorder
https://www.nimh.nih.gov/health/topics/schizophrenia

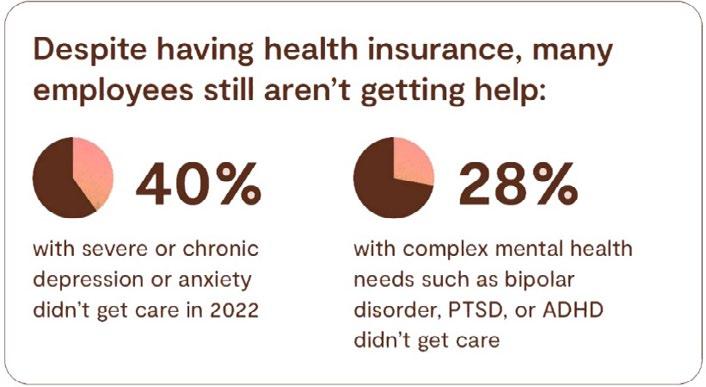
According to the 2023 State of Workforce Mental Health (Lyra) which surveyed more than 2,500 employees and more than 250 employee benefits leaders at companies in the United States with global workforces:
• Most workers face mental health struggles but, for myriad reasons, many don’t get help
• Many employees struggle to get the right care
• More people are discussing mental health at work, propelling a culture shift
• Managers lack needed mental health resources
• Employees are increasingly stressed and burned out, signaling a need for better work design.
Specifically, 86% faced at least one mental health challenge in the past year, ranging from issues like stress and relationship problems to chronic depression and anxiety, SUD and suicidal thoughts. Just 33% said they received mental health support last year, which includes seeing a therapist or psychiatrist, and using self-care resources such as stress reduction apps.
A TELUS Health survey showed that 21% of US employees are at high mental health risk and 42% are at moderate risk, but many people remain unaware of the mental health resources available to them through workplace benefit programs.
Paula Allen, global leader, Research and Total Well-being, TELUS, offers advice for plan sponsors and advisors to help employees and their families better cope with the current stressors.
She says, “Communication that workers can relate to, that includes advice on next steps and that is repeated often enough for them to remember, can help increase their use of available benefits. Members often do not know the range of resources available to them in their benefits packages and are often unaware of counseling included in the company’s employee assistance program.”
Source: 2023 State of Workforce Mental Health. Lyra Health
Adler calls out the lack of access to mental health providers through traditional channels (health plan network, EAP). “This has led employers to add multiple BH solutions to their mental health and wellbeing platforms. Adding BH navigational services to help guide employees and dependents to the right type of care quickly and seamlessly also “moves the needle” in satisfaction.”
The Society for Human Resource Management found that 78% of organizations currently offer or plan to offer mental health benefits this year, but utilization and accessibility are major hurdles for those seeking care.
Notably, six out of 10 adults who say their mental health is only fair or poor have not been able to access services, according to a 2022 survey from CNN and the Kaiser Family Foundation.
Studies confirm that the U.S. has a shortage of mental health providers and estimates are that the country will be short between 14,280 and 31,109 psychiatrists in the next few years.
This is problematic for employees who finally decide that they need help and may not be able to find it. Too often they get a list of doctors participating in the plan but discover that those doctors already have too many patients – or they don’t return calls in a timely manner and may not get back to them until a week later or longer.
Results of a study conducted by the Integrated Benefits Institute (IBI) on mental health concerns among employed adults ages 18-64 in the United States reveals that while employers have existing efforts to support mental health in the workforce, the pandemic greatly accelerated the progress of these efforts.
IBI researchers also report that because mental illness is often accompanied by other comorbid conditions such as diabetes and heart disease, providing options that help employees coordinate their care is important.
There is consensus regarding the importance of helping employees find mental healthcare that is culturally appropriate, that they value, and that they can identify with. All agree that adopting a prevention mindset for mental illness, as they do for physical illness, is a step forward.
Employees do care about mental health benefits. A new poll from the American Psychological Association Work and Well-being Survey reveals that 81% of employees would prefer to work for companies that provide support for mental health concerns.
The survey also reports that one-third of workers said their company’s mental health initiatives have improved since the pandemic began and 71% of respondents said they believe their employer is more concerned about employees’ mental health now than they were in the past.
In addition to mental health support, the PSA survey indicates employees would also like to see:
• more flexible work hours (41%)
• a culture that respects paid time off (34%)
• the ability to work remotely (33%)
• a 4-day work week (31%)
Increasing access to treatment is a key part of the solution. There is growing recognition of the value of BH integration (BHI), defined as the result of primary care teams (or teams in other care settings) and behavioral clinicians working together with patients to provide
Source: Integrated Benefits Institute
Driving better outcomes in partnership with:
Healthcare navigation, guidance and support with live concierge and an intuitive app
Here’s how:
Healthcare Navigation
Full-service population health, clinical and risk management solutions
• Easy mobile access to benefits information and ID cards
• Provider matching, price transparency and appointment booking

• Steerage to third-party solutions—saving time and frustration
Coordinated Care Management
• Proactive member engagement
• Integrated daily claims and pre-certification for cost-saving steerage
• Targeted clinical programs including discharge planning, high-risk pregnancies, pediatrics, and oncology
Join us June 6 th to learn more about how MedWatch is disrupting the status quo! Register today for the Premier Solution webinar.

At HPI, we’re staying ahead of high-cost claims by proactively steering members to quality, cost-effective care.
patient-centered care using a systematic approach.
It’s an approach to delivering mental health care that makes it easier for primary care providers to include mental and BH screening, treatment, and specialty care into their practice.
The CDC advises that the BHI approach enables the primary care provider to receive consultations by phone about a diagnosis and treatment plan from the care provider for mental health.
For example, practicing together in a co-location model, the primary care practice has a care provider for mental health practicing onsite who is responsible for screening and referrals and may provide therapy.
To improve referrals and communication, a care coordinator manages referrals to care providers for mental health and needed social services and maintains communication between the primary care practice and care providers for mental health.
BHI can result in better outcomes for children and youth, more efficient and coordinated care, higher treatment rates, reduced stress and improved consumer satisfaction.
According to a 2020 RAND study conducted in collaboration with the AMA, while physician practices had broad motivations for BHI, they faced multiple barriers to successful integration including cultural differences, incomplete information flow between behavioral and nonbehavioral health clinicians and billing difficulties.

Overcoming these barriers to BHI adoption is now possible through the introduction and adoption of tele-behavioral health or as the NIH National Institute of Mental Health terms this “tele-mental health”: the use of telecommunications or videoconferencing technology to provide mental health services.
Sometimes referred to as telepsychiatry or telepsychology, research suggests that tele-mental health services can be effective for many people, including, but not limited to those with attention-deficit/ hyperactivity disorder (ADHD), post-traumatic stress disorder (PTSD), depression, and anxiety.
Today, forward-looking healthcare organizations are integrating primary care and behavioral care services into one seamless care model.
Michael Brombach, COO, Recuro Health, says, “There is significant value when BH services are embedded with primary care. The impact spans lower costs, improved outcomes and better member experience scores. We thoughtfully designed and implemented our behavioral health solution to be a part of our core care model, enabling members to access the right level of both behavioral health and primary care services. Our capability navigates members to their primary care doctor, a counselor or a psychiatrist based on their conditions, history, and acuity.”
Telehealth has become a key driver to increasing access to behavioral health services. With growing patient demand and greater regulatory flexibility, adoption of tele-behavioral
“You have become a key partner in our company’s attempt to fix what’s broken in our healthcare system.”
- CFO, Commercial Construction Company
“Our clients have grown accustomed to Berkley’s high level of customer service.”
- Broker
“The most significant advancement regarding true cost containment we’ve seen in years.”
- President, Group Captive Member Company
“EmCap has allowed us to take far more control of our health insurance costs than can be done in the fully insured market.”
- President, Group Captive Member Company
“With EmCap, our company has been able to control pricing volatility that we would have faced with traditional Stop Loss.”
- HR Executive, Group Captive Member Company
People are talking about Medical Stop Loss Group Captive solutions from Berkley Accident and Health. Our innovative EmCap® program can help employers with self-funded employee health plans to enjoy greater transparency, control, and stability.

Let’s discuss how we can help your clients reach their goals.
This example is illustrative only and not indicative of actual past or future results. Stop Loss is underwritten by Berkley Life and Health Insurance Company, a member company of W. R. Berkley Corporation and rated A+ (Superior) by A.M. Best, and involves the formation of a group captive insurance program that involves other employers and requires other legal entities. Berkley and its affiliates do not provide tax, legal, or regulatory advice concerning EmCap. You should seek appropriate tax, legal, regulatory, or other counsel regarding the EmCap program, including, but not limited to, counsel in the areas of ERISA, multiple employer welfare arrangements (MEWAs), taxation, and captives. EmCap is not available to all employers or in all states.
health is only rising. Recuro’s BH solution is comprehensive and includes therapy, counseling, psychiatry and medication management, all offered through secure and private online video and phone sessions.
“Now, more than ever, Americans are struggling at home and work with mental health issues that fall under the behavioral health umbrella,” Brombach continues. “Consumer demand, along with physician appetite for new behavioral health models, enables virtual care companies to innovate in this space. Recuro’s care team model, culturally

intentional care approach and inclusion of optional pharmacogenomics for medication management are a few of the recent advancements we released to the market.”
As stigmas around mental health are subsiding, Brombach says that BH is becoming more accepted and accessed as part of its virtual care model, connecting patients and providers face-to-face in real-time as part of a virtual first approach to care.
“We look forward to continuing to innovate in this space to ensure individuals have access to the BH care they need, when they need it, at an affordable cost,” he concludes.
Adler also observes an increase in the use and offering of digital program delivery, adding, “Treatment of mental health disorders has shifted from primarily in-person care delivery models to digital models of care as a result of the COVID-19 pandemic. With more options for employees and for best clinical outcomes, treatment should be matched to the employee’s need and situation.”
She says that virtual visits may be best for employees who work shifts or want to have their treatment in the evening and for others, in-person services is preferred.
“Navigator Healthcare was founded to let employees engage with a 24/7 clinical Navigator to help guide them to the right level and setting of care based on their individual situation and personal preferences (virtual or in-person), assisting individuals with an evaluation appointment within 48 hours - saving the employee time and providing a seamless concierge experience,” she adds.
Mueller points to a partnership that Custom Design Benefits has with CuraLinc HealthCare and its SupportLinc assistance program.
“We implemented it for our own employees first and then introduced it to our clients at our 2022 Annual Customer Conference,” she explains. “Over 10% of our group clients have adopted the program since we rolled it out in early 2023 and we expect more to add the service on or before their annual renewal.”
She says that one plus is that Custom Design Benefits has its own Medical/Case Management services in-house.
The company’s nurses can educate members on the various resources the CuraLinc digital solution provides and refer them to a therapist covered under their health plan if they need additional assistance beyond the sessions covered at 100% with CuraLinc.”
As background, mental health parity describes the equal treatment of mental health conditions and SUDs in insurance plans.
In 2008, Congress passed the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) to ensure equal coverage of treatment for mental illness and addiction as they do with medical and healthcare-related benefits. benefits. The Affordable Care Act (ACA) also extended parity to non-grandfathered individual insurance plans and small group health plans.
Parity applies to quantitative treatment limitations (QTLs), for example restrictions on the number of days, episodes, or treatments that are covered and financial requirements, such as copays and coinsurance.
More recently, Congress expanded mental health parity law to also
include a parity analysis related to non-quantitative treatment limitations (NQTLs). This sixpart test creates documentation standards to ensure that the use of utilization review or prior authorization requirements are not more restrictive for BH benefits coverage than for other medical and surgical coverage.
A plan following the federal mental health parity law must cover equally the six classifications of benefits defined in MHPAEA final rules: (1) inpatient, in-network; (2) inpatient, out-of-network; (3) outpatient, in-network; (4) outpatient, out-of-network; (5) emergency care; and (6) prescription drugs.
Federal parity also applies to clinical criteria used by health insurers to approve or deny mental health or substance use treatment.
The standard for medical necessity determinations— whether the treatment or supplies are considered by the health plan to be reasonable, necessary, and/or appropriate—must be made available to any current or potential health plan member upon request. The reason for denials of coverage must also be made available upon request.
Here’s the challenge:
There are Issues surrounding NQTLs: the processes, strategies,
We study it, research it, speak on it, share insights on it and pioneer new ways to manage it. With underwriters who have many years of experience as well as deep specialty and technical expertise, we’re proud to be known as experts in understanding risk. We continually search for fresh approaches, respond proactively to market changes, and bring new flexibility to our products. Our clients have been benefiting from our expertise for over 45 years. To be prepared for what tomorrow brings, contact us for all your medical stop loss and organ transplant needs.

evidentiary standards, or other criteria that limit the scope or duration of benefits for services provided under the plan. In support of its members, SIIA has been involved in coalition and congressional discussions between mental health providers and employer groups.
Ryan Work, senior vice president, Government Relations, explains, “The entire NQTL requirement is vague, and SIIA is working hard to push the DOL to issue clarifying durance or model NQTL language to support and help with MHPAEA compliance. As noted above, MHPEA is a federal law that generally prevents group health plans and health insurance issuers that provide mental health or substance use disorder (MH/ SUD) benefits from imposing less favorable benefit limitations on those benefits than on medical/ surgical benefits.”
Work continues, “My understanding is that the DOL has yet to see an acceptable NQTL report at first pass. Not a single one. As the Report to Congress outlines, the Employee Benefits Security Administration (EBSA) has conducted nearly 90 investigations thus far, and issued hundreds of letters for comparative NQTL analysis.”
However, while the DOL has not seen an acceptable report, it has also not provided an example of what an acceptable one may look like. Hopefully, they will soon be updating the self-compliance tool.
In the meantime, the DOL has outlined a number of common NQTL shortfalls, including:
• Conclusory assertions lacking specific supporting evidence or detailed explanation
• Non-responsive comparative analysis
• Documents provided without adequate explanation
• Failure to identify the specific MH/SUD and medical/surgical benefits or MHPAEA benefit classification(s) affected by an NQTL
• Limiting scope of analysis to only a portion of the NQTL at issue
• Failure to demonstrate the application of identified factors in the design of an NQTL
By loosening limitations on telehealth during the pandemic and extending those flexibilities in Medicare in the FY 2023 omnibus bill, Congress has significantly elevated the successes of telehealth.
Legislative developments also continue to boost the use and expansion of telehealth as a critical component of rendering behavioral healthcare, including extended flexibilities in providing such care, removal of geographic restrictions, loosening of certain healthcare supervision requirements and extension of greater flexibility for prescribing controlled substances in connection with medication assisted treatment (MAT).
The MH/SUD stakeholder community applauds these moves and is now calling on Congress to make those flexibilities permanent.
Employees that request a leave to address their or their family member’s mental illness are protected under the US Department of Labor Family Medical Leave Act (FMLA) which is available to:
• Eligible employees: Employees are eligible if they work for a covered employer for at least 12 months, have at least 1,250 hours of service for the employer during the 12 months before the leave, and work at a location where the employer has at least 50 employees within 75 miles.
• Covered Employers: Private employers are covered employers under the FMLA if they employed 50 or more employees in 20 or more workweeks in the current or preceding calendar year, including joint employers or successors in interest to another covered employer. Public agencies, including a local, state, or Federal government agency, and public and private elementary and secondary schools are FMLA covered employers regardless of the
Medical Stop Loss from Berkshire Hathaway Specialty Insurance comes with a professional claims team committed to doing the right thing for our customers – and doing it fast. Our customers know they will be reimbursed rapidly and accurately – with the certainty you would expect from our formidable balance sheet and trusted brand. That’s a policy you can rely on. Reimbursement
right. www.bhspecialty.com/msl
number of employees they employ.
FMLA requires employers to:
• provide 12 work weeks of FMLA leave each year;
• continue an employee’s group health benefits under the same conditions as if the employee had not taken leave; and
• restore the employee to the same or virtually identical position at the end of the leave period.
• FMLA may be unpaid or may be used at the same time as employer provided paid leave.
FMLA also designates specific mental and physical health conditions for eligibility, including
if the employee requires inpatient care or ongoing treatment from a medical provider — severe conditions might include a hospital stay or seeking help at a treatment facility.
Often, employers require the medical provider — such as a psychologist or psychiatrist familiar with the person’s mental health history — to furnish a letter explaining the condition’s ability to encumber the employee.
The letter may also indicate whether a chronic mental health condition necessitates immediate, ongoing treatment.

In a turbulent domestic and world environment, improving mental health in the workplace is becoming a priority. Employers are beginning to emphasize employee well-being -- not simply as an obligation -- but as an opportunity to enhance productivity and retain top talent.
Going forward, mental health benefits are expected to become the norm with further regulations in place.
The escalating cost of providing prescription drug coverage is at the forefront of employers’ minds. Work with an experienced trusted partner who can help navigate this complex world. ELMCRx Solutions is that partner – Results Oriented, Accurate and Clinically Based.
“While there may be some generational differences in behavioral health stigma, it has declined significantly over the past decade across all demographics,” says Adler. “With the advent of ‘mental health days’, employers increasingly offering access to behavioral health tools and services beyond EAP and the media coverage of mental health issues/trends during the pandemic will continue to reduce stigma. Employers are able to directly reduce stigma in BH by offering access to more mental health solutions and discussing the importance of behavioral healthcare.”
Laura Carabello holds a degree in Journalism from the Newhouse School of Communications at Syracuse University, is a recognized expert in medical travel, and is a widely published writer on healthcare issues. She is a Principal at CPR Strategic Marketing Communications. www.cpronline.com
h ttps://www.benefitspro.com/2023/01/16/health-care-2023-what-doesthe-new-year-hold/ https://www.uhc.com/broker-consultant/news-strategies/resources/healthcare-trends-impacting-employers-2023
https://www.cms.gov/cms-behavioral-health-strategy
https://blog.telehealth.org/2023-preview-of-telemental-health-laws-
behavioral-telehealth-regulations/ https://www.polsinelli.com/ publications/polsinelli-top-issuesin-behavioral-health-2023newsletter
https://polsinelli.gjassets.com/ content/uploads/2023/02/ March_23_Behavioral_Health_ Newsletter.pdf
https://www.ama-assn.org/ delivering-care/public-health/whatbehavioral-health
https://www.ama-assn.org/ delivering-care/public-health/ compendium-behavioral-healthintegration-resources-bhi-basics
https://apibhs.com/2018/05/10/thedifference-between-mental-andbehavioral-health
https://www.uhc.com/brokerconsultant/news-strategies/ resources/health-care-trendsimpacting-employers-2023

https://www.healthline.com/health-news/over-80-of-us-workers-seek-employers-who-care-about-their-mentalhealth#What-the-APA-survey-shows
https://apibhs.com/2018/05/10/the-difference-between-mental-and-behavioral-health
https://www.ama-assn.org/delivering-care/public-health/behavioral-health-integration-physician-practices-randstudy
https://www.umassglobal.edu/news-and-events/blog/comparing-behavioral-health-vs-mental-health
https://www.nimh.nih.gov/health/publications/what-is-telemental-health#:~:text=Telemental%20health%20 is%20the%20use,to%20provide%20mental%20health%20services.
https://get.lyrahealth.com/whitepaper-2023-state-of-workforce-mental-health-report.html?utm_
source=google&utm_medium=paidsearch&utm_campaign=pa-2023-q1-search-google-2023-workforce-mentalhealth&utm_content=mental-health-state-2023&utm_term=mental%20health%20and%20work&campaignid= 14807085567&adgroupid=127227439345&adid=649605853108&gclid=CjwKCAjwitShBhA6EiwAq3RqA7ua1p5aM3iJR4i4axtW0cJLYtkNBJ1iKNmwSWwgg8XvlngdSQzJhoCtHsQAvD_BwE
https://www.benefitspro.com/2023/04/11/21-of-workers-at-high-mental-health-risk-and-unaware-of-availablecounseling/ https://lifeworks.com/en/media/1640/download?inline
https://www.dol.gov/agencies/whd/fact-sheets/28o-mental-health#:~:text=The%20Family%20and%20 Medical%20Leave,to%20address%20mental%20health%20conditions
https://www.benefits.gov/benefit/5895
https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/report-tocongress-2022-realizing-parity-reducing-stigma-and-raising-awareness.pdf
https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/mhpaeaenforcement-2021.pdf
https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-39-final.pdf
https://blog.nisbenefits.com/resources-finalized-for-mental-health-parity-compliance
https://www.dol.gov/agencies/ebsa/laws-and-regulations/laws/mental-health-and-substance-use-disorder-parity
https://www.benefitnews.com/news/how-to-design-mental-health-benefits-employees-will-use
https://pubmed.ncbi.nlm.nih.gov/29540118/
https://www.dol.gov/agencies/whd/fact-sheets/28o-mental-health
https://my.clevelandclinic.org/health/treatments/9301-antidepressants-depression-medication https://www.socialworkers.org/practice/clinical-social-work
https://www.mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health-providers/art-20045530
https://www.benefitnews.com/advisers/opinion/fmla-to-support-employee-mental-health?position=ed itorial_1&campaignname=V2_EBN_Daily_Views_20210421-02152023&utm_source=newsletter&utm_ medium=email&utm_campaign=V2_EBN_Daily_Views_20210421%2B%27-%27%2B02152023&bt_
ee=AzzLSdLf5k4I%2BkMW93l%2BTm1eA1XbFkLuNu9Zr5yHDuUXoZbX80NmPm8xhkQMPYRL&bt_ ts=1676494857901
https://www.cms.gov/cms-behavioral-health-strategy
https://www.managedhealthcareexecutive.com/view/aud-therapy-wins-fda-s-breakthrough-device-designation https://www.benefitnews.com/news/reminding-employees-about-their-mental-health-benefits-reduces-stigmaand-improves-engagement
https://healthpayerintelligence.com/news/top-5-common-conditions-driving-employer-healthcare-spending)
Staying healthy depends on being proactive. So does spend management. At Vālenz® Health, we believe lowering healthcare costs is driven by the ability to engage early and often in the member’s healthcare journey.

Before a claim even begins, we use data to identify cost, network and plan design opportunities to drive cost containment and improved health outcomes for members. We ensure everyone is aligned. There are no surprises – just reduced costs, better outcomes, and an improved member experience from start to finish.
That’s our promise to you. This is precisely why our customers stay with Valenz, because no one else does what we do.
See how Valenz engages early and often to deliver smarter, better, faster healthcare: visit valenzhealth.com or call (866) 762-4455.
 Proud to be a Diamond Member
Proud to be a Diamond Member
FROM TREATING EMAILS WITH CAUTION TO ENGAGING OUTSIDE EXPERTISE, ERECTING GUARDRAILS HAS BECOME NECESSARY FOR SELFINSURED PLANS
Written By Bruce ShutanAAs the workplace deepens its digital footprint and electronic medical records become the norm, efforts to shore up cybersecurity protection have become a necessary cost of doing business across the selfinsurance community.
Cybercriminals are increasingly mining health care data by making payers, providers and plans their top targets last year, according to a recently released report from Fortified Health Security. The number of medical record breaches increased to 51.4 million, which was up from 49.4 million the previous year, with more than 78% attributed to hacking and IT incidents. In addition, health care providers remain the overwhelming source of breaches, accounting for 70% of 2022 incidents.

Industry observers often say that these thieves are more sophisticated with their attacks, which is why cybersecurity protection is an area where expertise cannot be understated.

“My biggest recommendation would be to look for a very look for a good outside vendor who can support your company and meet with that entity once a month just to review their protocols,” says Mary Ann Carlisle, chief operating officer of ELMCRx Solutions, LLC, which assists selfinsured employers in managing their prescription drug benefits. “It’s an investment in your company and a lot less expensive than trying to build all of that inside your own organization.”
In keeping with ERISA’s fiduciary standard to act in the best interest of plan participants, PlanTools, LLC CEO David Witz explains that advisers must obtain on behalf of the plan sponsors they serve an annual due diligence report on cybersecurity for two reasons. One is that documentation demonstrates a fiduciary process. Also, it helps the commercial insurance carrier supplement its policy with the appropriate terms and coverage to protect employers from cybersecurity claims.
Like all benefit plan sponsors and administrators, self-insured health plan administrators are obliged to monitor and ensure that the recordkeeper has state-of-the-art cybersecurity protections in place, says Susan Rees, an attorney with extensive ERISA experience with the Wagner Law Group. But plans and plan fiduciaries also must be prepared to have their own cyber insurance policy to help mitigate these risks, she adds.
Liability for cybersecurity breaches may include civil or criminal penalties under the Health Insurance Portability and Accountability
Act, as well as litigation expenses related to participant claims for ERISA fiduciary breach or state privacy and security violations, notes Sarah Bassler Millar, a partner at Faegre Drinker.

Given how technology has evolved since HIPAA took effect in 1996 and in light of remote work’s increasing popularity, she advises plan sponsors to review their privacy and security policies and procedures. With so many working Americans logging into their laptops at home, local coffee shops or on the road, more personal data is now at risk for hacking than ever before.
There also are state and federal regulatory challenges to consider. “One of the problems is that the recordkeepers are subject to state law, and state privacy laws will give participants a cause of action against the recordkeeper where that same cause of action against the plan sponsor or plan fiduciaries is most likely preempted by ERISA,” Rees explains. “So recordkeepers are on the line for sure.”

Another obstacle is that there’s limited case law and the most noteworthy litigation involves retirement plan assets rather than health plans. All lawsuits involving cybersecurity breaches of employee benefits plan participant data or assets have been settled at the district court level, she notes. “So we don’t have any strong legal guidance on some of the issues,” she explains.
This void has been partially filled by the Department of Labor (DOL), which in April 2021 issued a dozen best practices that plan sponsors, fiduciaries, recordkeepers and participants can follow to reduce the risk of sensitive employee medical information falling into the wrong hands.
Although, it seems like the courts, and DOL are inclined to take the position that “when a recordkeeper’s computer system gets hacked, it’s the responsibility of that service provider to have provided an adequate service to the plan to protect the plan assets and plan data,” Rees says, describing the DOL guidance as good advice.
Among the noteworthy court cases, three involve lawsuits against Alight Solutions LLC, a cloud-based human capital and technology services provider. One of the first publicized cases of a cybersecurity breach in the employee benefits arena was
filed in April 2020. A U.S. district court judge presiding over Bartnett v. Abbott Laboratories dismissed claims against the plan fiduciaries involving the theft of $245,000 from the plaintiff’s retirement plan account, but allowed both ERISA and state law claims to proceed against Alight Solutions. The vendor was named as a defendant in a separate suit filed by a participant in Estee Lauder’s 401(k) plan over $99,000 in missing assets, which was settled in March 2020, and also subject to a DOL successful subpoena enforcement action in the Seventh Circuit.

Another case filed in July 2022 involving Alight that Rees says serves as a cautionary tale is Disberry v. Employee Relations Committee of the Colgate-Palmolive Co. et al. The plaintiff, a retired Colgate-Palmolive marketing executive named Paula Disberry, alleged a breach of fiduciary duty under ERISA after a cyberthief emptied more than $750,000 from her 401(k) plan.
With regard to this ruling, she says the judge seemed to suggest that the parties needed to figure out a way to pay the plan participant her money and greenlit the case for trial. “It’s almost like the judge was helping the participant to make her case, which is really not the job of a district judge,” according to Rees, who assumes this case will be settled.
While cyber thieves continue to crack complicated codes, they also know all too well the value of simple schemes of deception. One of the most underrated areas of cybersecurity breaches involves email, observes Michael Carrara, CEO of Hi-Tech Health, whose claims management platform is used by third-party administrators, carriers and provider-sponsored plans.
“People don’t understand an email is not secure by nature,” he says. “All it takes is a name associated with an address, date of birth and the first three of a Social Security number, and people can take out car loans, mortgages and credit cards. It’s really scary.”
“Fatima

“I've


The explosion of artificial intelligence is expected to further complicate cybersecurity protection. Carrara has little doubt that AI is becoming involved with “phishing” attacks that send fake emails or other messages that look like they’re from reputable companies. The purpose of this fraudulent activity is to induce individuals to reveal personal information such as passwords and credit card numbers. “I get bills from FedEx with the company’s logo and everything,” he reveals. “Sometimes the attacks are hard to decipher whether they’re real.”

One of the most recent hacking attempts Carrara has noticed involves what he describes as “brute force threats from these bad actors who are constantly trying to infiltrate through different holes in your firewall.”
Apart from having a dedicated department whose sole concern is cybersecurity, Hi-Tech Health relies heavily on its partners and tries to stay at the forefront of this topic through seminars and blogs. Other steps include moving all systems to a tier-one data center’s managed hardware platform whose firewalls are safely maintained and the company is constantly apprised of threats. Different layers of protection also allow Hi-Tech Health to take advantage of everything from Center for Internet Security protocols to expertise from in-house network engineers.
Carrara’s employees also undergo monthly online training with different scenarios and an annual penetration test from different third-party companies that supplements weekly penetration tests from Carson & Saint, a security and management consulting firm. In addition, Soc 1 and Soc 2 audits, which stand for service organizational control, are done to protect financial controls as well as security, processing integrity, confidentiality and privacy.
Cybersecurity compliance is difficult enough in the U.S., but those efforts expand even further when it involves overseas business. Since Hi-Tech Health’s client base is worldwide, for example, the company is subject to general data protection regulation rules in Europe, as well as HIPAA in the U.S.
Another protective layer that has become a table stake for self-insured employers and their partners is cybersecurity insurance, which Carrara says is mandatory in this climate, noting that his firm has $2 million in coverage for each incident. “It’s not only government that’s being attacked,” he explains. “It’s health insurance. It’s banking. It’s retail. Attacks are doubling.”

While perfect protection against cybersecurity breaches is always the goal, and the vast number of attacks are thwarted, the reality that some health plan sponsors and participants face can be harsh. Adds Rees: “Some of the human errors that have enabled hacking up to this point are fairly low level. There are hundreds, if not thousands, of attempts to hack into plans and service providers, and 99% of them are unsuccessful. All it takes is that 1%.”
Bruce Shutan is a Portland, Oregon-based freelance writer who has closely covered the employee benefits industry for more than 30 years.
Markel has developed a strategic collaboration with Nevaeh to provide new product solutions for employer accident and health coverage.
Nevaeh products have distinct advantages, but working together provides a leveraging effect that’s called the Nevaeh advantage which includes:

• Employer stop loss insurance
• Supplemental medical and accident insurance
• Outpatient, PBM carve-out plans
For more information, visit nevaehinsurance.com

Self-insured health plans and their vendor partners should be following these five steps to stay ahead of cyber thieves and protect highly sensitive personal information, suggests Mary Ann Carlisle, chief operating officer of ELMCRx Solutions, LLC. They include:
1. TFA or MFA: Two factor authentication, or TFA for short, will send a code to one’s smartphone whenever a password is changed, which must be entered in order to access an online account. When two or more steps are required every time someone logs into a system, it’s called multi factor authentication, MFA for short.
2. VPN or VDI: Securing work conducted in a virtual personal network known as a VPN or virtual desktop interface known as VDI will keep information private and secure. Working through a cloud or server-based system that requires entering an email address and password that generates an authentication code is safer than logging into a computer’s local drive, which creates a risk if the computer is lost or misplaced.
3. Public facing: Information that is stored on a company website is considered “public facing” content made available to the general public. It can be easily obtained by cyber thieves who break into the back end of a website. Medical information stored in the VDI is more safely contained in that ecosystem and is not public facing.
4. Scanned attachments: One of the most basic cybersecurity efforts involves scanning attachments for malware and viruses before making them available to recipients to be safely opened. Advanced threat protection scans attachments for these threats and ensures that any Word, Excel, PowerPoint, etc. documents are legitimate.
5. Phishing tests: Monthly phishing tests, along with mandatory training on this issue, will help walk users opening attachments or clicking on embedded links and how to spot red flags. One such example is when the sender’s email address doesn’t match up with the organization that is being impersonated to poach personal information. Any cyber threats should be documented and included in a monthly report to the cybersecurity carrier.
At

•
•
•
•
•
•
•
•
•
•
 Written By Caroline McDonald
Written By Caroline McDonald
TThe rising prices of goods and services, healthcare, wages, increasing litigation and the lingering effects of pandemic supply chain issues, are impacting companies across the nation, contributing to inflation.
According to U.S. Labor Department data published February 14th, the inflation rate for the United States for a range of goods and services rose by 6.4 percent for the previous 12 months, down slightly from a rate of 6.5 percent in 2022.
Rising wage costs and higher prices could impact key metrics used for measuring performance of captive insurance programs, including loss rates and claim frequency, explained Amy Angell, Principal & Consulting Actuary at Milliman in Chicago.
“Higher claim costs, particularly in property and some liability lines of business, have resulted in the need for higher captive funding levels,” she said. “And the effect of inflation is still making its way through open liability cases.” She added that captives writing liability coverages need to monitor their experience and assess reserve levels on an ongoing basis.
Because captives are part of a larger risk management program that includes commercial excess insurance partners,
and repairs as well as greater involvement of plaintiff attorneys.
“Social inflation and attorney advertising is affecting a broad array of coverages,” she said. Those include employment practices liability, professional liability, construction liability, and premises liability for high-traffic retail operations.
Maryellen Vargas, consulting actuary at Milliman in Chicago notes that employers using captives may have greater incentive, “to implement programs that can help manage claim costs and therefore combat inflation.”
She noted that no industry is immune from the effects of inflation. The impact on an individual organization depends on “the mix of operations insured, and the coverages offered through the captive,” she said. “Certain operations, such as commercial trucking and property exposures, have seen cost increases across industries.” Organizations that have experienced labor shortages and high employee turn-over may be seeing a greater inflation impact, Angell said.
One line of coverage seeing heavy impact from inflation is automobile.
“The auto line of coverage is a standout,” said Sandra Springer, senior vice president, director of marketing for Captive Resources, in greater Chicago. “Inflation rates applicable to new vehicles, and parts and equipment, since Jan. 1, 2020, were up 14-15 percent. In the fourth quarter of 2022, they were significantly outpacing overall inflation rates,” she said.
Angell noted that the climb of commercial auto liability, auto physical damage, and property coverages is due to higher costs of materials
Angell added that captives are a valuable part of an overall risk management strategy, as using a captive to its maximum, “means continually reviewing the coverages and coverage limits being offered through the captive.”
Tracking and understanding the impact of inflation on exposure bases is important, she said.
For example, “payroll may be increasing due to higher average hourly wages, sales may be increasing due to inflation, and total insured value may be increasing with higher property valuations.” Increases in the exposure bases, “may not correlate one-to-one with expected increases in insured costs,” Angell said.
“Many single-parent captives have increased their policy limits to accommodate higher retentions and to help make the overall insurance program more cost effective,” Angell said.
The captive also should evaluate its own premium rates to ensure that they are reflective of the current average inflation level of the exposure bases. “And if the commercial market has increased premium rates ahead of loss trends, or not adjusted for the anticipated effect of the inflationadjusted exposure bases, this may represent an opportunity for the captive to offer higher coverage limits,” Angell said.

Medical inflation on average is higher than general inflation. Milliman reports in its white paper, “Medical Inflation: Drivers and Patterns,” that two trends emerge:
• Medical inflation patterns often, but not always, follow a similar but lagged pattern to general inflation.
• Annual medical inflation tends to be higher than its general counterpart (1.7 percentage points higher, on average).
Inflation, Vargas said, is impacting most parties involved in the U.S. healthcare system – from providers to health plans and employer plan sponsors.
Healthcare inflation is driven largely by rising costs on the provider side, “that flow through the rest of the healthcare system,” Vargas said. The causes are similar to those in other sectors, including increasing labor costs, supply costs, and other operational costs. An added component is the high costs often attached to emerging healthcare treatments and technologies, she said.
“We primarily see the impact of inflation on healthcare unit cost trend,” she said.



Vargas added that while the impact of healthcare inflation on those employers that purchase healthcare may not differ significantly by industry, “One key differentiator will be the provider reimbursement structure inherent in the provider network being accessed,” she said.
Networks that have reimbursements based on Medicare’s payment structure or on negotiated fixed fee amounts, such as per diems or per admission payments for hospitals, “will be less impacted by healthcare inflation than networks whose reimbursement is calculated as a percentage of billed charges,” Vargas said.
“The best claim remains the claim that does not happen,” Angell said. “Investment in safety and risk management programs that address the root causes of claims can help to lower both the frequency and severity of claims.”
Another strategy is to align the captives with the incentives of the insureds. “For example, increasing member deductibles in a group captive program or adjusting the internal charge-back program for a single-parent captive,” can help in achieving better adoption

of important safety and risk management initiatives, she said.
Also helpful is more frequent monitoring of loss experience, which can help alert captive management to changing trends in the data, “and to avoid surprises at year-end,” Angell explained.
Because captives may have experienced declines in invested asset values in 2022, reviewing capital adequacy levels is an important step in the financial management of the captive, “particularly in light of the greater volatility that may have been introduced with the addition of new coverages or higher policy limits,” she added.
The Insurance Information Institute reports in its study, Group Captives: An Opportunity to Lower Cost of Risk:
Participation in a group captive can help companies save on insurance costs and provide access to extensive risk management resources, including industry-specific expertise. These attributes are a source of value in the best of times, and today’s inflationary conditions may increase their appeal for certain types of companies.
Attention to risk management and safety is important for member companies with a goal of keeping their losses lower within the captive retention, said Sandra Springer, senior vice president, director of marketing for Captive Resources in greater Chicago. This can “help to lower their individual premiums since those are based on the member company’s own loss experience,” she said.
Springer noted that an industry hit hard by inflation is construction. “Worker shortages, higher materials costs, supply chain interruptions and housing shortages are among the issues impacting the industry and contributing to rising prices,” she said.
Construction is also, “the largest industry segment among the group captives we support – there are over 2,000 construction companies across the U.S. in our client captives,” she said, adding that demand for group captive insurance remains high in this sector, “as a long-term cost management solution.”
Inherent features of the group captive model help member company insureds to continually drive down costs, she explained. “The model focuses companies on risk management and safety and provides them with numerous services and resources to support their efforts,” Springer said.
The typical result is lower losses, “which results in lower costs over time from lower premiums and dividends received for better-than-expected loss performance,” she said.

Some of the group captives have also increased their primary limits. “This all helps to control the captive’s excess insurance cost – at a time when excess insurance costs have been increasing exponentially in the marketplace,” Springer said.
Caroline McDonald is an award-winning journalist who has reported on a wide variety of insurance topics. Her beat has included in-depth coverage of risk management and captives.
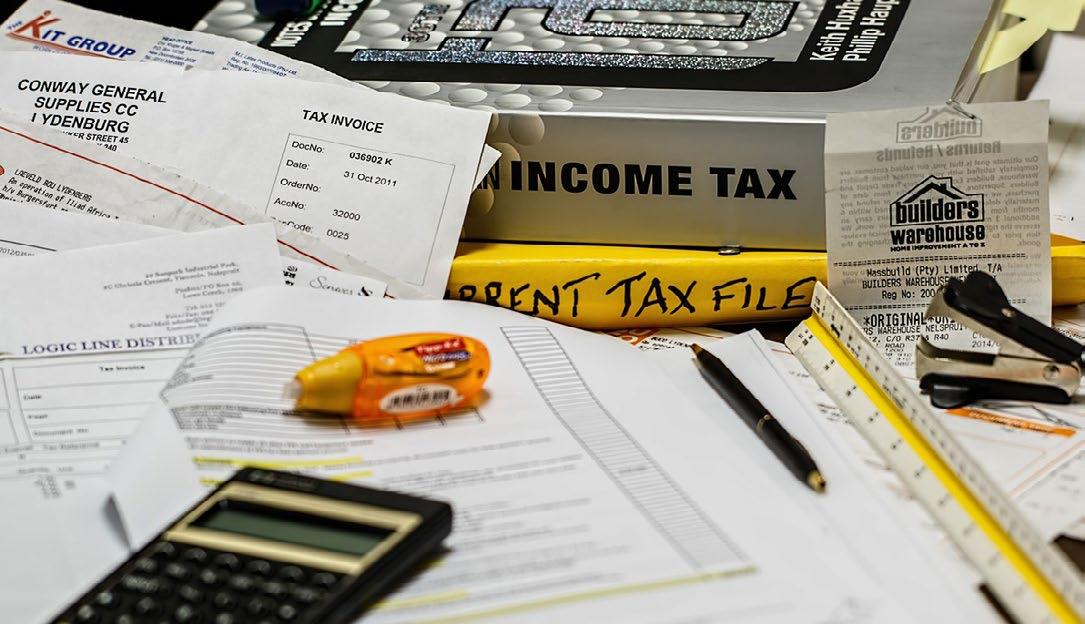
TheAffordable Care Act (ACA), the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and other federal health benefit mandates (e.g., the Mental Health Parity Act, the Newborns and Mothers Health Protection Act, and the Women’s Health and Cancer Rights Act) dramatically impact the administration of self-insured health plans. This monthly column provides practical answers to administration questions and current guidance on ACA, HIPAA and other federal benefit mandates.
Attorneys John R. Hickman, Ashley Gillihan, Steven Mindy, Carolyn Smith, Ken Johnson, Amy Heppner, and Laurie Kirkwood provide the answers in this column. John is partner in charge of the Health Benefits Practice with Alston & Bird, LLP, an Atlanta, New York, Los Angeles, Charlotte, Dallas and Washington, D.C. law firm. Ashley and Steven are partners in the practice, and Carolyn, Ken, Amy, and Laurie are senior members in the Health Benefits Practice. Answers are provided as general guidance on the subjects covered in the question and are not provided as legal advice to the questioner’s situation. Any legal issues should be reviewed by your legal counsel to apply the law to the particular facts of your situation. Readers are encouraged to send questions by E-MAIL to John at john.hickman@alston.com.
The IRS recently released internal guidance from its Office of Chief Counsel to the head of its employment tax policy division that reiterates and emphasizes the potentially severe consequences of taking shortcuts when substantiating flexible spending account claims (IRS Chief Counsel Advice 202317020, March 29, 2023, released April 28, 2023.
Employers, TPAs, and card processors must ensure that they follow the IRS substantiation rules as written without administrative shortcuts like sampling, de minimis thresholds, or other methods that do not satisfy the IRS substantiation guidelines set forth in the IRS Notices and proposed regulations. Otherwise, FSA plans risk disqualification of the entire cafeteria plan.
As the IRS memo makes clear, if the cafeteria plan is disqualified then all non-taxable benefits any employee receives through the employer’s cafeteria plan must be included in gross income and are wages subject to withholding for Federal Insurance Contributions Act (FICA) and Federal Unemployment Tax Act (FUTA) purposes.
In other words, the consequences of failing to adhere to the IRS guidelines extend to defeat all tax advantages employers and employees receive via a cafeteria plan and are not limited to the improperly adjudicated claims.
The IRS memo does not break new ground or add any new rules. The IRS’ Office of the Chief Counsel prepared it for the IRS’ head of employment tax policy.
It’s unlikely the IRS will make an official statement about what prompted the memo, but the memo indicates that the IRS does not agree with interpretations that the Internal Revenue Code (“Code”) or IRS guidance allow certain substantiation practices that have been become more common for reasons such as administrative convenience or cost reduction.
The IRS’ memo provides five examples of impermissible substantiation practices, but the IRS’s position is not limited to these five examples and likely extends to additional methods that do not adhere to IRS guidance:
1. Self-certification -The IRS memo notes that all claims must be substantiated under the Code and IRS guidance. Accordingly, self-certification of claims that are not otherwise substantiated does not fulfill the requirement that every FSA claim must be substantiated by information from a third-party party that is independent of the employee and their spouse and dependents (Notice 2006-69). The IRS memo notes that its prior guidance prohibits self-substantiation of medical expenses (Prop. Reg. § 1.125-6(b)(3)). As a result, the cafeteria plan is disqualified if it
only requires an employee to submit information describing the service or product, the date of sale or service, and the amount, but does not also require a statement from an independent third party to verify the expense.
2. Sampling – A cafeteria plan is disqualified if it reimburses all debit card charges but requires the employee to substantiate with thirdparty information a random sample of debit card charges that were not otherwise auto-substantiated under IRS rules. The IRS notes that its guidance requires substantiation of all claims (either manually or in accordance with IRS autoadjudication guidance) and prohibits the use of sampling techniques (Prop. Reg. § 1.125-6(b); Rev. Rul. 200343).
3. De minimis thresholds – A cafeteria plan is disqualified if it does not require substantiation of all debit card charges (either manually or in accordance with IRS auto-adjudication guidance) regardless of how small the expense is. Plans must limit reimbursement and claims payment to medical expenses substantiated with third-party information that describes the service or product and includes the date of the service or sale (which the IRS notes includes expenses that are autosubstantiated consistent with IRS guidance) (Prop. Reg. §
You want unparalleled customer service. Employers need the right stop loss coverage. At Swiss Re Corporate Solutions, we deliver both. We combine cutting-edge risk knowledge with tech-driven solutions and a commitment to put our customers first. We make it easy to do business with us and relentlessly go above and beyond to make stop loss simpler, smarter, faster and better. We’re addressing industry inefficiencies and customer pain points, moving the industry forward – rethinking employer stop loss coverage with you in mind.
corporatesolutions.swissre.com/esl
1.125-6(b); Notice 2006-69; Notice 2003-43).
4. Favored providers – A cafeteria plan is disqualified if it does not require employees to substantiate debit card charges (either manually or in accordance with IRS auto-adjudication guidance) even though they may be incurred at certain providers whose expenses almost always qualify (e.g., dentists, doctors, hospitals, or other health care providers). As in the other examples, the plan must require substantiation of all claims (including via IRS approved auto-adjudication methods) and plans cannot exclude claims incurred
at specific providers or facilities from their substantiation requirements. Note that real time adjudication or EOB rollover procedures for such providers are still allowable as long as they satisfy existing IRS guidance.

5. Advance Dependent Care Assistance Claims – A cafeteria plan is disqualified if it pays or reimburses an employee’s dependent care expenses by submitting a form before receiving the dependent care that attests to the amount of dependent care expenses they will incur in the upcoming year. A plan cannot cure this by requiring employees to provide an after-the fact notice if their dependent care situation changes and they will not incur the qualified dependent care expenses to which they attested. The IRS reiterates that dependent care expenses paid by debit card must be substantiated with a statement from the dependent care provider that includes the dates and amounts for dependent care services provided (Prop. Reg. § 1.125-6(g)). Additionally, the IRS reminds plans that dependent care expenses cannot be reimbursed before the expense is incurred (Prop. Reg. § 1.125-6(a)(4)). A dependent care expense is incurred when the care is provided and not when the employee is formally billed, charged, or pays for dependent care.
We deliver value other TPAs can’t match. Our three-year medical trend is beating the industry at 2.6%, our claims reviews are finding an extra 15% in savings before network discounts, and our Excellent NPS Score tells us we’re keeping our clients very happy. Our people deliver incredible value for our customers. They can do it for you too.
As for consequences, the IRS says that employers sponsoring health FSAs that use the methods described in the first four examples must include all reimbursements by the health FSA during the year in the gross income of employees, including claims that were substantiated consistent with IRS guidance.
The IRS adds that an employer providing the advance reimbursement of dependent care expenses must include all payments under the dependent care assistance plan in the gross income of employees and wages of employees for FICA and FUTA tax purposes.
Perhaps even more significantly for employers, the IRS adds that its flexible spending accounts’ failure to follow the substantiation requirements in Prop. Reg. § 1.125-6(b) is also a failure to operate in accordance with the written plan or a failure to operate in accordance with Code § 125 and § Prop. Reg. § 1.125-1(c)(7)(ii)(G).
This supports the IRS’ position that the entire cafeteria plan is disqualified by substantiation failures and the tax consequences are not limited to the flexible spending accounts. Thus, even employees who do not make an FSA election will lose the pre-tax advantages under the employer’s cafeteria plan.
In addition to the amounts that an employer must add to income and wages if its cafeteria plan is disqualified, the employer also becomes liable for applicable penalties and interest payable to the IRS for reporting and withholding errors and might need to amend its prior returns and reports, including employees’ W-2s.
In other words, the consequences are potentially far reaching and could reverberate across an employer and its workforce when a flexible spending account uses substantiation methods that the IRS has not adopted in its guidance.

AAs advancements in how individuals consume healthcare have drastically and rapidly improved (i.e., the prevalence of virtual patient care, online pharmacies where treatments can be received and delivered to the home, etc.) face-to-face communication between providers and patients has often been supplanted by virtual interactions that expedite processes. The result is faster and easier access to healthcare.
Improved access is certainly a step forward, but is it enough? For patients diagnosed with a rare or life-threatening condition where the only treatment is difficult to obtain, the answer is probably not.

Availability is a challenge for patients seeking gene and cell therapy as treatment can cost millions to obtain. Cost is a factor and has the potential to impact the availability of treatment for patients. Access and availability are not always in parity when it comes to patient care.
Research shows and common sense would suggest that providing healthcare services for patients to maintain or restore their physical, mental, or emotional well-being is best when the patient care is embedded with empathy and kindness; it greatly enhances the healing process. Compassion is important for healthcare providers, and for employers with self-funded healthcare benefit plans.
Gene and cell therapies are quickly evolving, and employers need to understand the potential impact. Employers face the tall order of exuding empathy while relating to employees contemplating the multimillion-dollar treatment that is gene and cell therapy.
Even the most compassionate of such professionals find it difficult to strike the delicate balance of weighing costs to their respective plans with the natural inclination to provide coverage for potentially lifesaving or life-altering therapy.
Knowledge and a solid game plan for how to manage gene and cell therapy within their plan design, however, will allow employers to confidently focus their energy on the employee facing life-threatening circumstances instead of being blindsided by the economics of the situation. By understanding the nuances and limitations, plan sponsors should be well-positioned to employ a strategy that uniquely balances compassion and cost.
The following discussion highlights some of the plan administration and documentation considerations for employers navigating the evolving gene and cell therapy landscape.
According to the FDA, gene therapy is a method that modifies a person’s genes to treat or cure disease, while the American Society of Gene + Cell Therapy (ASGCT) defines cell therapy as the transfer of live cells into a patient to treat or cure a disease -- i.e., a blood or marrow transplant is a type of cellular therapy.
Undoubtedly, accessibility and attainability are challenges for patients and plan sponsors as they learn more about cell and gene therapies, which has been a very hot topic in recent years. The response to these innovative treatments has been mixed: The medical community is advocating the new treatments for patients hoping to find a cure for their respective rare diseases while health plans remain concerned about potential costs.
In the past couple years, the pipeline of both pending and U.S. Food & Drug Administration (FDA) approved treatments has grown. In fact, in January 2019 FDA Commissioner Scott Gottlieb noted the surge in cell and gene therapy products entering early development and predicted that the FDA would be approving 10 to 20 cell and gene therapy products a year by 2025 based on the assessment of the current pipeline and clinical success rates.
Flash forward to the present day and as of April 2023, the FDA has (according to fda.gov) approved over 25 cell and gene therapy products. Furthermore, according to the Alliance for Regenerative Medicine (ARM), there could be as many as 13 brand new cell or gene therapies approved in the United States, Europe, or both by the end of 2023, and there is a large queue of various clinical trials for gene and cell therapies listed on the ClinicalTrials.gov website.
Why is there so much excitement over these developments? Gene and cell therapies potentially offer a new avenue for treatment in cases where there were otherwise limited options for such rare and life-jeopardizing diseases.
Indeed, some of the FDA approved cell and gene therapy treatments on the market have yielded curative changes with a one-time treatment. Long term metrics and results are still being examined, but as the interest
in and education about these types of treatments increases, employers who sponsor selffunded health plans should take the opportunity to decide how to address such coverage within their plan designs.
Many factors should be considered by employers as they navigate this new landscape.
For example, if a treatment is approved for use in Europe, but not in the United States, would such benefit be eligible for coverage under the current plan design (if the individual travels to Europe) or is there an exclusion for foreign travel (i.e., benefits received outside the United States if travel is for the sole purpose of obtaining medical services)?
Even if plans have the strictest language possible for international medical tourism, how does the plan currently address gene and cell therapy? Is there an exclusion? Is there a benefit? Are there limits? Is the plan silent?
This is an important conversation as cutting-edge science and technology continue driving forward the current state of medicine in the United States, and the queue for more FDA approved gene and cell therapies is rapidly growing.
While it’s undeniable that these advancements in treatment options can come with an overwhelming price tag, the conversation becomes more nuanced when further questions are considered: What if covering the one-time treatment could potentially cure the condition and offset the need for other expensive ongoing or lifelong care? Further, if the plan did cover such benefits would they be reimbursable by the plan’s stop loss carrier? Are there alternative payment options?
Plans, however, are still permitted (and should) ensure benefits are covered subject to the appropriate medical management techniques. For example, plans should have a strong definition and policy for how medical necessity is determined. The plan should also review the definition of experimental and investigational to ensure the language is in line with its expectations. Other plan options may include precertification or prior authorization requirements on the benefits.
A key question plans may be asking is what they are required to cover. The Affordable Care Act (ACA) prohibits plans from imposing dollar limitations on any of the 10 categories of essential health benefits (EHB). To the extent the plan covers an EHB, no dollar limitations may apply to that benefit. Self-funded plans should have identified a particular state benchmark to which they determine and classify EHBs under the plan design.
In 2022, HHS released the 2023 final payment rules which provide that for plan years beginning on or after January 1, 2023, an EHB plan design should be clinically based, among other factors.
Further, in late 2022, HHS published a request for information (RFI) asking for public comment by January 31, 2023, regarding a variety of topics, but including the description of EHBs and questions involving the barriers to accessing services due to cost, coverage and whether EHBs needed to be updated to account for changes in medical evidence or scientific advancements.
The timing for plan design changes should be considered as well. Plan design modifications should comply with the ACA and ERISA timing requirements and may be best incorporated at plan renewal to mitigate discrimination concerns.
Consequently, coverage and access issues remain pressing issues. Plans should be mindful when it comes to their decision-making surrounding how and whether to extend (or limit) coverage for gene and cell therapy. These are tough choices for employers and plan sponsors, and they need support as they weigh the various factors and considerations to make an educated decision.
As gene and cell therapies develop so too are the options for plan sponsors when it comes to potential payment methodologies. Traditional health plans were not structured to handle one-shot, highcost treatments so alternative options are important to consider.
For example, new reinsurance programs are emerging to offer options for plans hoping to cover gene and cell therapies. Each of these programs is unique and should be reviewed against the existing plan materials to ensure the program aligns with the intentions of the plan sponsor and the terms of the plan document/summary plan description.
Patient support programs where patients receive support for cell and gene therapy may also be available. Unlike traditional drug patient assistance programs, these programs may offer psychosocial, economic, and caregiver assistance to the patients and their families.
The support programs may be individualized to address clinical issues and matters involving logistical and transportation related support, financial support, and nurse navigation support.
Other payment strategies could include multiple year payment plans, reimbursement based on meaningful outcomes or performance-based measures for the treatment, payment model where the price reflects the value, or a methodology that includes a warranty (where a refund may be issued if the treatment fails after a certain time).
In adopting a strategy for coverage (or exclusion, or limited coverage) of gene and cell therapies, plan sponsors should balance the various factors. While there may not be a perfect solution, plans need a strategy that is clearly consistent with plan materials so there is no confusion among plan participants (or between other contracts held by the plan sponsor).
For example, in navigating this evolving area of benefits, plan sponsors should ensure the plan document/summary plan description aligns with their coverage decision; the stop loss policy provisions are free from conflict with the underlying plan materials; review any potential supplement programs that may assist in the coverage of these gene and cell therapy benefits; continually monitor the regulations as state and federal laws regarding price transparency and drug pricing pass to ensure ongoing compliance; and keep abreast of the pipeline of pending and newly approved FDA therapies.
New (and costly) gene and cell therapy treatments are on the horizon. As a result, it will be important for employers to have the appropriate balance between tight controls to ensure patients see the value and benefit of these high-cost treatments. Having a strategy that successfully connects employees and plan members with life-changing treatments and mitigates the financial impact, while demonstrating compassion, is critical.
Jennifer M. McCormick joined The Phia Group, LLC in 2008. As the Senior Vice President of Phia Group Consulting, Attorney McCormick concentrates on a variety of healthcare and regulatory issues facing employee benefit plans and their administrators while also focusing on health benefit plan regulatory compliance services, including but not limited to selffunded health plan consultation, health plan exclusions, health plan limitations, health plan revisions, definitions of key items such as usual and customary fees, and the entire health plan summary plan description and summary of benefits and coverage. She is a constant contributor to The Phia Group’s webinars and other educational media.
Attorney McCormick earned her J.D. from the Syracuse University College of Law, with certificates in Estate Planning and Family Law, and her B.A. in both Psychology and Criminal Justice from Indiana University, graduating with distinction as a National Dean’s List Scholar. While attending Syracuse, Attorney McCormick served as an Intercollegiate Director of the Moot Court Honor Society and as a Student Attorney in the Low-Income Taxpayer Clinic where she counseled clients on state and federal tax matters and the U.S. Tax Court appeals process.
SIIA Diamond, Gold, and Silver member companies are leaders in the self-insurance/captive insurance marketplace. Provided below are news highlights from these upgraded members. News items should be submitted to membernews@siia.org.
All submissions are subject to editing for brevity. Information about upgraded memberships can be accessed online at www.siia.org.
If you would like to learn more about the benefits of SIIA’s premium memberships, please contact Jennifer Ivy at jivy@siia.org.










PHOENIX, AZ — In its commitment to protecting highly sensitive information for customers and partners, Vālenz® Health has attained SOC 2 Type 2 audit certification, which significantly minimizes risk of data breaches and other costly vulnerabilities.
SOC 2 Type 2 reports are the most comprehensive certification within the SOC protocol.
To obtain certification, Valenz underwent a rigorous, long-term audit from an independent third-party auditor licensed by the American Institute of Certified Public Accountants. The audit examines the design of internal controls and the operating effectiveness of data security systems to verify adherence to these high standards.
“In our increasingly data-driven world, cybersecurity is among the top concerns for every company. It is essential that we provide the highest level of data protection for our customers, and they deserve transparency into how we achieve that for true peace of mind,” said Rob Gelb, Chief Executive Officer of Valenz. “Our attainment of SOC 2 Type 2 certification aligns with the Valenz culture of trust and demonstrates our ability to keep customer data private, safe and secure.”
Vālenz® Health simplifies the complexities of self-insurance for employers through a steadfast commitment to data transparency and decision enablement powered by its Healthcare Ecosystem Optimization Platform. Offering a strong foundation with deep roots in clinical and member advocacy, alongside decades of expertise in the validation, integrity and accuracy of claims, and a suite of risk affinity solutions, Valenz optimizes healthcare for the provider, payer, plan and member. By leveraging data transparency and delivering an omnichannel approach across the healthcare journey, Valenz improves cost, quality and outcomes for employers and their members – engaging early and often for smarter, better, faster healthcare. Visit www.valenzhealth.com
Kavita Reddy is a highly accomplished technology leader with a proven track record of success spanning over 20 years in the healthcare sector. Kavita has consistently delivered innovative solutions that have resulted in significant improvements to healthcare cost containment.
During her tenure at Zelis, Kavita played a key role in driving the company’s growth and success. She successfully implemented several state-of-the-art solutions in healthcare cost containment, reference-based pricing, and claims processing.
Kavita also led critical application modernization, data transformation and digital transformation initiatives involving artificial intelligence and machine learning.
“We were seeking the right technology leader to help drive our future. We selected Kavita after an extensive search process involving many excellent candidates. Kavita stood out due to her impressive technology experience in healthcare cost containment and strong cultural alignment with our core values. She will be a great asset as a leader for our company, and

By supporting people in the moments that matter, we can improve health outcomes and help employers manage costs.
For over 40 years, self-funded employers have trusted Sun Life to help them manage financial risk. But we know that behind every claim is a person facing a health challenge and we are ready to do more to help people navigate complicated healthcare decisions and achieve better health outcomes. Sun Life now offers care navigation and health advocacy services through Health Navigator, to help your employees and their families get the right care at the right time – and help you save money. Let us support you with innovative health and risk solutions for your business. It is time to rethink what you expect from your stop-loss partner.
Ask your Sun Life Stop-Loss Specialist about what is new at Sun Life.
The content on this page is not approved for use in New Mexico. For current financial ratings of underwriting companies by independent rating agencies, visit our corporate website at www.sunlife.com. For more information about Sun Life products, visit www.sunlife.com/us. Stop-Loss policies are underwritten by Sun Life Assurance Company of Canada (Wellesley Hills, MA) in all states except New York, under Policy Form Series 07-SL REV 7-12. In New York, Stop-Loss policies are underwritten by Sun Life and Health Insurance Company (U.S.) (Lansing, MI) under Policy Form Series 07-NYSL REV 7-12. Product offerings may not be available in all states and may vary depending on state laws and regulations. © 2023 Sun Life Assurance Company of Canada, Wellesley Hills, MA 02481. All rights reserved. Sun Life and the globe symbol are trademarks of Sun Life Assurance Company of Canada. Visit us at www.sunlife.com/us. BRAD-6503-y SLPC 29427 01/22 (exp. 01/24)
we are thrilled to have her join the team. “ –
Matt Yost, Chief Executive OfficerEnsure Fairness and Transparency in Healthcare. We set healthcare free from the constraints of traditional models and outof-date billing practices. With our clinical expertise, industry experience, and proprietary evidence-based technology, we help solve some of the most complex issues in healthcare. Visit www.6degreeshealth.com
Nova has appeared on this distinguished list for six consecutive years
Buffalo, NY – Nova Healthcare Administrators was recently named one of the 2023 Best Companies to Work for in New York. Recognized for the sixth year in a row, Nova ranked 12th out of 28 finalists in the medium size company category.
This statewide survey and awards program is designed to identify and honor the best places of employment in New York, benefiting the state’s economy, its workforce and businesses.
Winners were honored at an awards ceremony on April 19 in Albany, where rankings were also announced. The 2023 Best Companies to Work for in New York list is made up of 75 companies across small, medium and large categories.
“I am so proud that Nova was named to the Best Companies list for the sixth year in a row,” said Nova’s President James Walleshauser. “This honor acknowledges the positive work environment of our organization and strong sense of community among our associates – who continue to make Nova a great place to work year after year. We work hard to foster a culture where all our associates are happy, healthy, engaged and empowered to speak up and be themselves. We believe that people who love the work they do, do work that people love.”
Whether meeting a client deadline or getting together for a Nova Navigators hike at a local park, Nova associates work hard and have fun. A variety of associate-led groups, including a Diversity Council, Renovations wellness committee and Nova in the Neighborhood volunteer and giving committee offer the opportunity to connect with one another, grow and make an impact on the company and community.
The annual Best Companies awards program is presented by the New York State Society for Human Resource Management (NYS-SHRM), Best Companies Group and BridgeTower Media/ Rochester Business Journal.
Companies from across the state entered the two-part survey process to determine the Best Companies to Work for in New York.
The first part consisted of evaluating each nominated company’s workplace policies, practices, and demographics.
The second part consisted of an employee survey to measure the employee experience.
The combined scores determined the top companies and the final rankings.
For more information on the Best Companies to Work for in New York program, visit www.BestCompaniesNY.com.
NOVA HEALTHCARE ADMINISTRATORS AWARDED 2023 PLATINUM BELL SEAL FOR WORKPLACE MENTAL HEALTH FROM MENTAL HEALTH AMERICA
BUFFALO, NY - Nova Healthcare Administrators has been awarded
Reaching compliance and transparency doesn’t have to be challenging. When it comes to staying abreast of the future regulations of the No Surprises Act, let Integrated Payor Solutions give you an ALL-ENCOMPASSING SOLUTION.
Transparency + is the most efficient and inexpensive solution to meet all current and future regulations of the No Surprises Act.
The Deadline for ALL Items and Services for Self-Service Tools Is January 1, 2024.
Is Your Compliance Solution Equipped to Meet Those Requirements?
The Bell Seal certification recognizes employers who strive to create mentally healthy workplaces for their employees, with platinum serving as the highest level of distinction. This is the second year in a row Nova has earned the Bell Seal.
In order to receive this prestigious designation, Nova underwent a rigorous evaluation of its policies and practices in four areas: workplace culture, benefits, compliance, and wellness programs.
Nova received an overall score of 90 out of 100, with a perfect 100 percent for workplace culture and wellness programs.
“Health is at the forefront of what we do and that starts with our own associates,” said James Walleshauser, president, Nova. “We take pride in providing resources, benefits and a work culture that support our associates’ overall wellbeing, including their physical, social, mental and emotional health. In a hybrid working environment, we’re committed to ensuring our associates feel connected, engaged and supported – and we are working hard to find innovative ways to accomplish that. So, we are honored to receive the Bell Seal for

Workplace Mental Health once again because it affirms our continued efforts and belief that if we take care of our associates, they will take care of our customers and one another.”
Nova’s receipt of the Bell Seal for Workplace Mental Health reflects not only the company’s commitment to wellbeing from its leadership, but the efforts of its associate-led wellness committee, called Renovations.
As part of a focus on overall wellbeing and intentional connections, in 2022 the committee launched a hiking club, the Nova Navigators, to promote associate engagement and joyful movement.
A first-of-its-kind healthcare SuperApp for self-funded plan sponsors that helps members make better decisions around quality medical care delivery, so everyone wins.
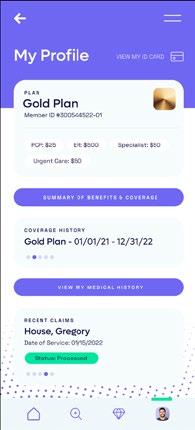
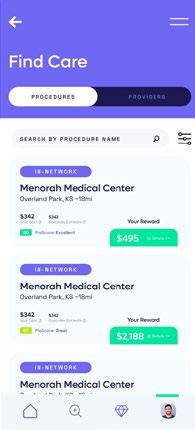
The only self-funded healthcare engagement platform of its kind.
Hercules Health rewards habitual app utilization by giving cash incentives earned through intelligent healthcare shopping tied to quality and cost. More app use equals more savings for members and plan sponsors alike.
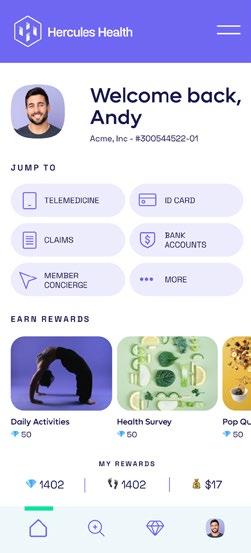
Hercules Health delivers best-in-class price transparency that is fully compliant with the Transparency in Coverage (TiC) and the No Surprises Act (NSA) rules and regulations.
Nova also strives to support associates through flexible working arrangements, regular company-wide meetings and internal communications, as well as a robust total rewards package that includes numerous mental and behavioral health resources.
To learn more about the Bell Seal for Workplace Mental Health, visit www.mhanational.org/ bestemployers.
Founded in 1982 and headquartered in Buffalo, NY, Nova is one of the largest third-party administrators of self-funded employee benefit programs in the nation, providing the health care solutions our clients need in the way they need them. And we go far beyond the basics. We are creative problem solvers who build custom solutions. Nova provides a customizable, comprehensive array of services, including medical, dental, vision, COBRA, reimbursement account administration, and private-labeled solutions. Nova also offers awardwinning, in-house, integrated medical management programs. We are the stewards of our clients’ benefit plans, offering best-inclass partnerships, customized solutions, and personalized service. Nova is a wholly-owned affiliate of Independent Health.
Mental Health America - founded in 1909 - is the nation’s leading
community-based nonprofit dedicated to addressing the overall mental health of all. MHA has spent decades researching mental health in the workplace, and in 2019, MHA introduced the Bell Seal for Workplace Mental Health to recognize companies and organizations that understand the value of addressing mental health at work and implement policies and practices that support employee wellbeing.
Concord, MA – Strategic Risk Solutions (SRS), the world’s largest independent insurance company manager, announced that Ron Sulisz has been appointed to the role of President of the global firm, a position he will assume effective May 15, 2023. He will report to Brady Young, who will remain as CEO of the company. Mr. Sulisz will also serve on the Board of Strategic Risk Solutions, Inc.
“As we continue to grow and expand, I recognized we needed more focus and resources to support operations and Ron will be perfect to lead this effort and focus on the corporate side of SRS, heading up the internal financial, operations, human resources, and information technology teams. It will allow me to focus more on strategy and supporting our operating units and ensuring we maintain our customer focus,” said Mr. Young.
Mr. Sulisz has been with SRS for 18 years and is currently CEO of SRS Cayman, having helped establish SRS as the leading captive manager in the domicile. Jenny Pooley will be assuming the role of CEO in Cayman.
“I’m excited for this new chapter at SRS, and although I will be shifting responsibilities to Jenny, I’m remaining in the Cayman office, and available to my clients and the relationships that I’ve built over my years at SRS,” said Sulisz.
As Ms. Pooley steps into her role as CEO of the SRS Cayman operation, she’ll focus on the management and supervision of client accounts, including financial and regulatory reporting and special assignments related to SRS’ captive management program in the Cayman Islands.
“Jenny has shown amazing leadership and knowledge in her 13 years at SRS Cayman,” said Mr. Sulisz. “She will transition very naturally into this role and the team in Cayman are excited for her in this new opportunity.”
risks with the industry’s most predictive and trusted risk score, making it easier than ever to see more stop loss risks and opportunities— and competitively price plans across your spectrum of underwritten groups.
SRS is the world’s largest independent insurance company manager. With over 25 years’ experience, SRS provides management and consulting services to a wide range of insurance company structures, from single parent captives to complex commercial insurers and reinsurers. SRS has operations in the United States, Europe, Barbados, Bermuda, Canada, Cayman Islands, and South Africa. Visit www.strategicrisks.com
Winston-Salem, NC – ACS Benefit Services announced that Bruce Allen will assume the role of Chief Executive Officer, effective July 1, 2023.
Allen, a health care industry leader bringing 25+ years of experience, will succeed Beverly Proctor, Interim CEO, who will resume her role as Chief Operating Officer on that same date.
Following his leadership of the implementation of the ACA for Blue Cross and Blue Shield of North Carolina, Allen was named their Vice President of Medicare.
His first-hand experience in product sales, retention and product development from the individual market, and small market to large national employers enables effective leadership coupled with an understanding of market shifts.
Under Allen’s leadership, Blue Cross NC’s Medicare membership increased by 50 percent over the past two years, while Star ratings increased from 3 to 4.5 stars. These impressive results were driven by member focus, service area expansion, a new suite of benefits, and audience targeted marketing.
The same member driven approach is found at ACS. Allen’s deep knowledge of product design, channel management and large implementations will be of great value to the company.
“Bruce is a well-respected and proven leader who has produced strong results across his tenure at Blue Cross NC. We are excited to see him step into this role to drive ACS’s continued strong performance.” said Matt Garabrant, ACS Board Chair.
Due to his deep knowledge of North Carolina and the health care industry, coupled with a leadership record of results, Allen’s selection as ACS’s new CEO brings the needed background to drive growth and
serve ACS’ distinctive clientele.
“ACS brings important capabilities, deep relationships and crucial market insights as we look to help employers meet the challenges of providing affordability, quality health benefits to their workforces,” Allen said. “I’m excited about the unique opportunities to provide third-party administration services to employers, who are looking for greater opportunity for the affordability and benefit flexibility ACS provides in the self-funded market.”
Allen received his bachelor’s degree in economics from Wake Forest University and his master’s in health care administration from UNC Chapel Hill. He currently resides with his family in Chapel Hill, NC.
At ACS Benefit Services, our sole focus is providing the most innovative products and services available in the health benefits marketplace—all backed with the highest level of customer support. Over the past four decades, we are proud to have grown into a leading third-party administrator (TPA) by continuously focusing on the future of the industry and creating long-term health plan solutions for our employer groups. Contact Beverly Proctor, Chief Operating Officer at www.bproctor@ acsbenefitservices.com and visit www.acsbenefitservices.com




























LAKE FOREST, Ill -- Bill Gould has joined national employee benefits provider Trustmark in the newly created role of President and Chief Operating Officer, reporting directly to Chief Executive Officer Kevin Slawin. As Trustmark advances growth strategies in each of its three businesses, Gould brings broad industry experience and expertise in key areas.
Gould joins Trustmark after nearly three decades at Securian Financial Group, a mutual holding company with revenue of $6.2 billion. He will relocate from Minneapolis to the Lake Forest area.
“Bill will be an important addition to an already strong leadership team at a time when Trustmark is poised to invest in and further expand our offerings in valuable
voluntary benefits, self-funded health plan design and administration for smaller companies, and virtual and in-person corporate and community fitness management solutions,” Slawin said. “He has extensive experience in customer-focused product development, partnerships and acquisitions, digital innovation, and large-scale strategic execution. Just as important, his career working for a mutual company and his values are an ideal fit with our mutual-company structure and caring culture.”
In his 27 years at Securian, Gould took on leadership roles of increasing responsibility, most recently as Executive Vice President for Affinity Solutions, a business focused on providing financial protection to millions of customers across the U.S. and Canada. There, he played a key role in digital transformation and strategic expansion, including the successful completion of several acquisitions.
Gould earned his MBA and BS degrees from the University of Minnesota Carlson School of Management. He serves on the Board of Directors for the Twin Cities Habitat for Humanity.
Trustmark, through its operating divisions and subsidiaries, offers specialized expertise in voluntary benefits, self-funded health plan design and administration for smaller employers, and in-person and virtual corporate and community fitness solutions. Trustmark’s commitment to building long-term, trusted relationships helps people, businesses, and communities thrive. Trustmark: benefits beyond benefits. Visit us at www.trustmarkbenefits.com

Ringmaster Technologies’ pharmacy consulting platform presented by its wholly owned subsidiary, “Ringmaster Rx”, is a huge win for Brokers, TPAs, and PBMs (pharmacy benefits managers). Its cloudbased data warehouse integrated with a RFP workflow process gives clients the ability to:
• Solicit, Compare and Award PBM Contracts and Programs
• Perform contract reconciliations & audits on contract performance
• Deliver sophisticated analytics and generate value added reports
• Customize their own panel of preferred PBM’s
• Efficiently manage cost for their employer groups

CHAIRWOMAN OF THE BOARD*
Elizabeth Midtlien
Vice President, Emerging Markets
AmeriHealth Administrators, Inc.
Bloomington, MN
CHAIRMAN ELECT & TREASURER AND CORPORATE SECRETARY *
John Capasso
President & CEO
Captive Planning Associates, LLC
Marlton, NJ
DIRECTOR
Stacy Borans
Founder/Chief Medical Officer
Advanced Medical Strategies
Lynnfield, MA
DIRECTOR
Matt Kirk President
The Benecon Group
Lititz, PA
DIRECTOR
Mark Combs
CEO/President
Self-Insured Reporting
Greenville, SC
DIRECTOR
Shaun L. Peterson
VP, Stop Loss
Voya Financial
Minneapolis, MN
DIRECTOR
Amy Gasbarro
Chief Operating Officer
Vālenz
Phoenix, AZ
DIRECTOR
Adam Russo CEO
The Phia Group, LLC
Canton, MA DIRECTOR
Deborah Hodges President & CEO Health Plans, Inc.
Westborough, MA
Captive Insurance Committee
Jeffrey Fitzgerald
Vice President
Innovative Captive Strategies
Waukee, IA
Future Leaders Committee
Erin Duffy
Director of Business Development
Imagine360
Wayne, PA
Price Transparency Committee
Christine Cooper CEO aequum, LLC
Cleveland, OH
Captive Insurance Advocacy Task Force
Jeffrey K. Simpson
Partner
Womble Bond Dickinson (US) LLP
Wilmington, DE
Workers’ Compensation Committee
Shelly Brotzge
Regional Underwriter, Group Self Insurance
Midwest Employers Casualty
Chesterfield, MO
SIEF BOARD OF DIRECTORS
CHAIRMAN
Nigel Wallbank
Preisdent
Leadenhall, LLC
Ocala, FL
PRESIDENT
Daniél C. Kimlinger, Ph.D.
CEO
MINES and Associates
Littleton, CO
DIRECTORS
Freda Bacon
Administrator
AL Self-Insured Workers' Comp Fund
Birmingham, AL
Les Boughner
Chairman
Advantage Insurance Management (USA) LLC
Charleston, SC
Alex Giordano
Chief Executive Officer
Hudson Atlantic Benefits
Bellmore, NY
Virginia Johnson
Strategic Account Director
Verisk/ISO Claims Partners
Charlotte, NC
* Also serves as Director
Paula Greve Director, Self-Insurance
Compliance
Aon Global Risk Consulting
Minneapolis, MN
John Ventura Director of Education
Spine Care Partners, LLC
Algonac, MI
Geoffrey Adamson CEO
ARC Fertility
Cupertino, CA
John Quinn Chief Executive Officer
Wellnecity
Winston-Salem, NC
We would like to invite you to share your insight and submit an article to The Self-Insurer! SIIA’s official magazine is distributed in a digital and print format to reach 10,000 readers all over the world.
Jeff Swearingen Co-Founder and Managing Director
Edgemont Capital Partners New York, NY
Elizabeth Freesmeier VP, Marketing Sharecare
Atlanta, GA
Robert Lang Managing Director
SL Management Partners LLC
Beverly, MA
Ryan O’Mahoney
Chief Operations Officer
Warrior Cost Management LLC
Glendale, AZ
The Self-Insurer has been delivering information to top-level executives in the self-insurance industry since 1984.
Articles or guideline inquires can be submitted to Editor Gretchen Grote at ggrote@ sipconline.net
The Self-Insurer also has advertising opportunties available. Please contact Shane Byars at sbyars@ sipconline.net for advertising information.


Catastrophic claims can arise unexpectedly. If the plan has the right Stop Loss protection in place, focus can remain on achieving business goals and welcoming Leo back when it’s time. When you work with the experts at HM Insurance Group, you can have confidence that the claims will be paid. Find more on hmig.com